Chronic Inflammation – Is that all there is to disease?
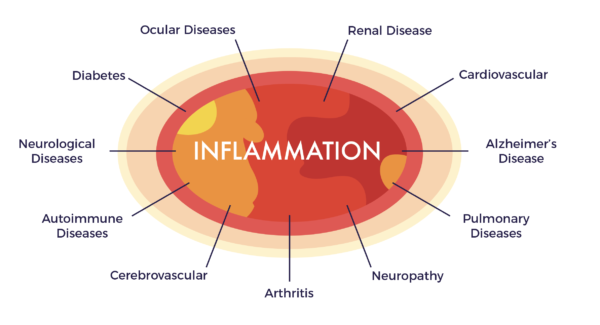
Chronic systemic inflammation (CSI) is a hot topic. This is for good reason as it is nearly universally agreed that CSI is a culprit in all chronic diseases of aging.
Major media outlets like the Washington Post and New York Times have featured stories on CSI. Raw and Red-Hot, summarized some of Harvard Medical School’s (and their affiliated institutions) enlightening studies on the subject.
By accessing the stem cells (and other regenerative cells) in our fat (adipose tissue), under the auspices of the Federal Right to Try Act of 2017, those with debilitating chronic systemic inflammatory conditions have access to a new option to improve their quality of life. You can read more about the Right to Try Act here.
But is inflammation all there is to it?
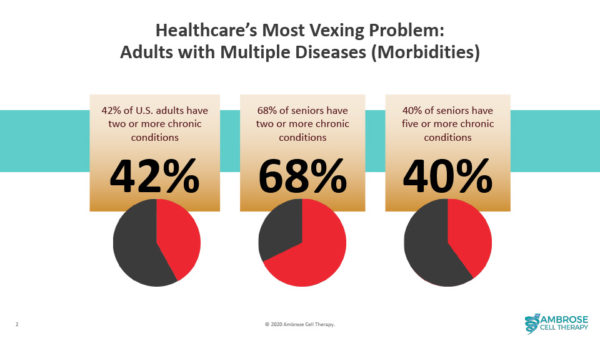
The intense focus on chronic inflammation (also known as “inflammaging”) has, in many instances, served to deemphasize (or even ignore) the other factors that are also commonly involved in chronic diseases. More on that in a moment; first the story of inflammation and the largely untold story of the biggest unmet need in healthcare – patients with multiple chronic diseases.
Inflammation
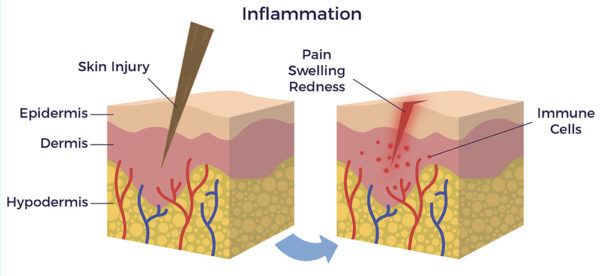
Inflammation isn’t a new idea. It has a long and colorful story. Egyptian papyri from almost 5,000 years ago refer to heat and redness as naturally associated with disease. From another angle, in the 5th century BC, Hippocrates described the beneficial side of inflammation as an early component of the healing process after tissue injury.
Put in everyday terms, short-term increases in inflammation (acute) are critical to repair, and even survival, in the event of physical injury and infection, respectively.
However, it has been revealed that certain social, environmental, trauma-related and lifestyle factors can cause inflammation to go out of control and become chronic. Chronic inflammation is like a smoldering fire inside the body; it slowly spreads, often igniting multiple chronic diseases (morbidities). Patients with multiple morbidities represent the most vexing problem in healthcare.
Given the broadscale recognition of the detrimental effects of inflammaging, there is an irrepressible movement in healthcare (including patients) to do something about it. Conventional doctors prescribe drugs to suppress inflammation, while integrative physicians recommend diets and supplements to tamp it down. Increasingly people (from the “worried well” to the chronically ill) drink green juices and eat kale salads to replace the sugary drinks, bread and desserts they were previously “enjoying” at the expense of their health.
Not to be left out, scientists are researching the pathways and genes in the body that turn excess inflammation on with the hope of discovering small molecules that can be put in a pill to turn it off like a light switch.
But, regardless of all that – and even with some people reporting benefits – the onslaught of chronic diseases of aging has not been reversed nor the prescriptions of drugs, surgeries and devices to fight them slowed.
The Plus Side
On the plus side, for more than 20 years hundreds researchers have described in more than 10,000 peer-reviewed papers, that a mixed population of stem and regenerative cells found in our fat (adipose tissue) can not only improve inflammatory markers, but also address the multiple factors that contribute to the ill health that resulted from inflammaging.
In 2016, researchers summarized the science and studies supporting the unique attributes of ADRCs in a review paper, Autologous Adipose Derived Regenerative Cells: A Platform for Therapeutic Applications.
Trish’s remarkable patient-reported outcome for “hypermobility”, an inherited connective tissue disease, is a profound example of the potential of benefits of AMBROSE Cell Therapy. Her condition had resulted in chronic inflammation, debilitating pain and disability. Unlike others in her family with the same condition, Trish is now able to live life to the fullest. Here is her story.
