Patient Reported Outcome – Amy
 In 2014, at the age of 24, my quality of life was rough. I had lived with Type 1 diabetes for 22 years already. I mismanaged my diabetes in college and, as a result, was in chronic, debilitating pain after developing neuropathy. After researching the science of stem cells, I decided to try cell therapy. I was treated with the stem cells and other regenerative cells residing in my fat, or adipose tissue. That one out-patient procedure marked a turning point in my battle. I am now six years out, living the life I want, and in much better control of my diabetes.
In 2014, at the age of 24, my quality of life was rough. I had lived with Type 1 diabetes for 22 years already. I mismanaged my diabetes in college and, as a result, was in chronic, debilitating pain after developing neuropathy. After researching the science of stem cells, I decided to try cell therapy. I was treated with the stem cells and other regenerative cells residing in my fat, or adipose tissue. That one out-patient procedure marked a turning point in my battle. I am now six years out, living the life I want, and in much better control of my diabetes.
Living with diabetes requires discipline. For most of my life, I was required to test my sugar levels, count carbs, and eat appropriately. By the time I went to college, I had diabetes, “burn out”. At one point, I stopped testing my blood sugars and just went with how I felt. That non-compliance landed me in the hospital for six weeks and brought on neuropathy and fibromyalgia that burned out of control. After that, I got my act together, but you could hardly call my life normal, even for a person living with diabetes.
When I was first diagnosed with neuropathy, my life consisted of sitting in a bathtub for 6 hours a day, running cold water over my feet. With medication, I got to a point where I could go to work, but constant pain and worry about when the next flare-up of even more intense pain dictated my life.
In my feet, I suffered from severe, chronic pain that caused a burning, tingling sensation twenty-four seven. It felt like someone took a hot poker, shoved it into the middle of my foot, and then vibrated the poker constantly.
You can’t imagine what it is to live like that. Walking or standing for too long was painful. Flare-ups of intense burning, swelling, or tingling controlled my life. I couldn’t sleep with a blanket. Just the graze of a sheet would set my feet off. I can’t even calculate the amount of sleep I lost. Just to get to sleep, I had to shake the bed to distract myself from the pain. Wearing shoes was a challenge, and socks could set a flare-up in motion. Even sneakers, which you would think would be comfortable, could sometimes be excruciating.
Fortunately, my dad suggested I look into whether adipose-derived stem and other regenerative cells could improve my neuropathy and help me bring my diabetes under better control.
The University of Missouri had just published a paper explaining how adult stem cells could restore blood flow to the pancreas. The increased blood flow improved insulin-producing cells’ function. Though it was a study done on mice, the science made sense to me. I had been following stem cell science for a while and was always interested in the possibilities. Plus, I was a little overweight, so getting liposuction in the bargain was a no-brainer as far as I was concerned!
My family was all for moving forward. They had seen me crying in the bathtub way too much not to be.
In the months leading up to cell therapy, sitting in a bathtub for six hours wasn’t really possible. I was working at that time – and living with four roommates. However, if it were super bad, I would sit on the edge of the tub and have the water run over my feet for long periods – which made said roommates “love” me. Even when on medication and “functioning,” the pain was debilitating because it was a constant physical drain and a psychological one. My feet had a constant dull ache. I could never be comfortable in my own body and was always worried about when I would get a flare-up.
On November 16, 2014, I received cell therapy with my adipose-derived regenerative cells (ADRCs). The protocol included IV infusion of clinical-grade ADRCs and direct injections in my feet to address the neuropathy.
 Several months after my treatment, I went for a regular check-up. Before cell therapy, I was at an HBA1C of 8.9, and after my reading was at a 7.8. Talk about happy: I had not been that low in years. My healthcare provider was thrilled at the AIC decline.
Several months after my treatment, I went for a regular check-up. Before cell therapy, I was at an HBA1C of 8.9, and after my reading was at a 7.8. Talk about happy: I had not been that low in years. My healthcare provider was thrilled at the AIC decline.
My symptoms of neuropathy and fibromyalgia improved over time. At about six months, I realized a full day had passed, and I had not thought about my feet once. That was absolutely shocking and utterly mindblowing to me. As cool as that was, at nine months, I started playing soccer, my favorite sport as a kid.
When your daily life is so affected by illness or pain that even mundane tasks are a challenge, it is not only debilitating physically but also psychologically. It limits one’s ability to dream.
Growing up, experiencing other cultures was ingrained in my sister and me by our parents. Travel was one of my favorite things to do. When you’re worried about the ability the walk down your own street, imagining walking the streets of another country seems insurmountable.
 Nearly a year after my stem cell therapy, I was able to take my first big trip to Greece. Not only was I able to walk the Oia trail in Santorini with my mom, but I was also able to try a special type of pedicure in which tiny fish nibble at your feet. Someone who hadn’t even been able to sleep with a sheet touching their feet was able to sit for a prolonged time and have fish nibble at their feet? Unimaginable and yet, it was possible!
Nearly a year after my stem cell therapy, I was able to take my first big trip to Greece. Not only was I able to walk the Oia trail in Santorini with my mom, but I was also able to try a special type of pedicure in which tiny fish nibble at your feet. Someone who hadn’t even been able to sleep with a sheet touching their feet was able to sit for a prolonged time and have fish nibble at their feet? Unimaginable and yet, it was possible!
Since the trip to Greece, I have traveled to Spain, Vietnam, and Iceland. Hiking the Grand Canyon was another major milestone.


I am now six years out from treatment. The defining moments marking my improvement came over many months. In the years since I have been to numerous countries with varying terrains. I got my daily life back, and also one of my most favorite things to do was possible again. I could dream again. As I look back, my improved quality of life is amazing compared to where I started, particularly when you consider that I have not done special diets or other strictly controlled measures.
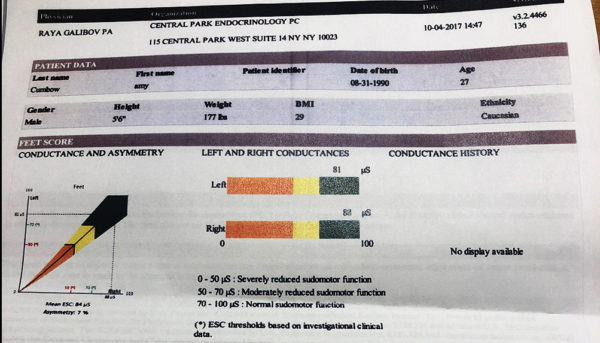
In 2017, my endocrinologist did Sudo Scan, a conductivity test that measures neuropathy. Per the results, my feet do not show damage associated with neuropathy.
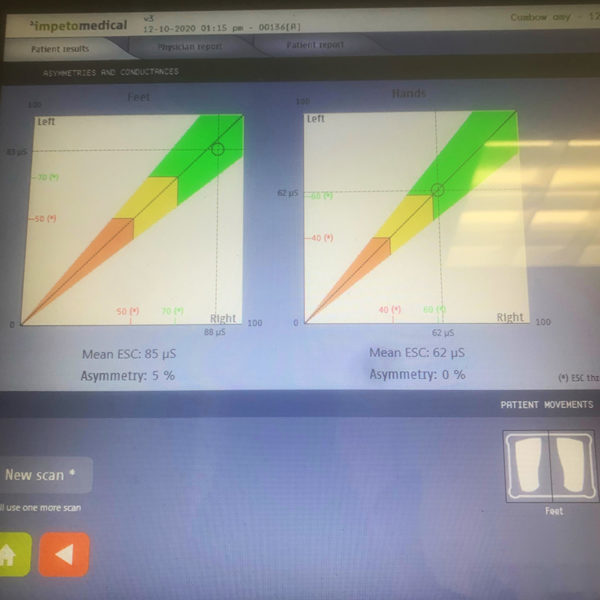
My diabetes specialist repeated the test in Dec 2020 with nearly identical results.
Admittedly, after cell therapy, I had some periods where I could have done better at testing. Though not nearly as bad as before, it wasn’t good for my A1C. However, I have learned from being a diabetic that tests only tell part of the story. Even with being somewhat lax from time-to-time, my chronic 10-point foot pain and fibromyalgia flare-up regularity was a night and day difference. Each person’s physiology is different, and it can change from moment-to-moment. If I get stressed and my sugars spike, my symptoms can flare up a bit. But the flare doesn’t last long or prevent me from living life. And, those flare-ups are tolerable.
In terms of testing my blood sugars, I am now on a continuous glucose monitor connected to an automated insulin pump. The two devices talk to one another. Knowing the minimum amount of insulin required to manage normal daily blood glucose fluctuations and my sugar level trend has helped me immensely. This information and the correct dosing of insulin based on that data were the missing pieces to better manage my blood glucose levels to where they were after cell therapy.
Today, I live and work full time in New York City. I am happily married and planning a family. I am in much better control of my diabetes.
 I am working in sales for an innovative diabetes technology company to help others control their diabetes. Being on my feet is a big part of my job. I am too busy working to play soccer; instead (before COVID), I worked out with a trainer twice a week, yet another thing that would not have been possible prior to my stem cell therapy.
I am working in sales for an innovative diabetes technology company to help others control their diabetes. Being on my feet is a big part of my job. I am too busy working to play soccer; instead (before COVID), I worked out with a trainer twice a week, yet another thing that would not have been possible prior to my stem cell therapy.
Here is how I look at it: Could I walk around Union Square? Could I go camping with friends? Could I walk across the Brooklyn bridge? Could I stand in heels for a meeting? Those were the types of questions that plagued me before. Now I do all those things without the psychological burden I previously had.
Cell therapy marked the turning point that led me to where I am now.






