Improving Cell Therapy Outcomes
Stress, inflammation, immune system dysregulation and both acute and chronic disease have been shown scientifically to be highly correlated. The activities of adipose-derived stem and regenerative cells (ADRCs) are well established to reverse the physiologic and biologic effects of stress that lead to or perpetuate the illness. If you complement your treatment by maintaining an appropriate stress level for your physical condition and age as well as removing inflammatory factors in your diet and lifestyle, your cell therapy benefits should be enhanced.
Inflammation and Stress
Research on the incidence and prevalence of disease increasingly suggests that exposure to traumatic stressors and psychological trauma is related to the onset and perpetuation of specific diseases as well as premature death.
Stress comes in more than one flavor, including:
- Emotional or psychological, such as financial, family or social issues, both short and longer-term in nature
- Physical trauma from an accident or acute event.
- Poor diet, lack of exercise and insufficient sleep
- Bad lifestyle habits such as smoking or substance abuse
The body responds to the various types of stress in both healthy and unhealthy ways via:
- Immune cells and signaling proteins release called cytokines. There are many different types of cytokines but here we are most interested in those that are supposed to initiate healthy inflammation (pro-inflammatory) and those that are supposed to reduce it (anti-inflammatory) when inflammation goes out of control.
- The endocrine system releases the hormone cortisol, which is also responsible for helping the body respond to stress by reducing inflammation and the abnormal immune response to stress.
You could think of pro-inflammatory and anti-inflammatory cytokines like the fire department that starts controlled burning to manage wildfire risk. As an example, we experience fever in response to an infection, or pain in response to an injury. These pro-inflammatory cytokines are meant to start ridding the body of infection or repairing the wound from the injury. At a certain point the fire needs to be put out so the fire department brings in the firehoses to douse the flames with water and things return to normal. Anti-inflammatory cytokines are like the water used to stop the fire.
Cortisol works in the opposite sequence. It is responds to the inflammation by reducing it, but it can over respond causing more stress and inflammation. In other words, it is there to support the firefighting cytokines, but cortisol can be too much of a good thing if the fire starts to burn out of control. In other words, excess stress on the body can lead to higher-than-normal levels of cortisol, which can result in cellular damage and decreased life expectancy.
The Cycle of Stress
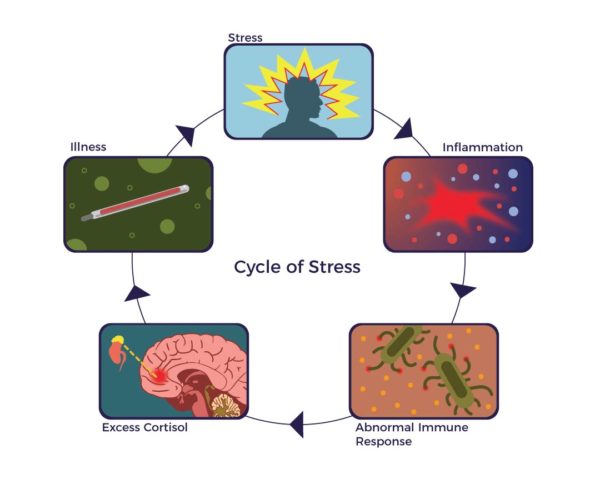 Many studies support the role that stress has in initiating and perpetuating the full range of acute and chronic illnesses and the role inflammation plays in symptoms, function and quality of life. Stress and abnormally high levels of inflammation have been tied to heart disease, neurological and autoimmune diseases. These factors initiate and perpetuate a negative cycle of both acute and chronic disease:
Many studies support the role that stress has in initiating and perpetuating the full range of acute and chronic illnesses and the role inflammation plays in symptoms, function and quality of life. Stress and abnormally high levels of inflammation have been tied to heart disease, neurological and autoimmune diseases. These factors initiate and perpetuate a negative cycle of both acute and chronic disease:
In two studies involving the common cold, Carnegie Mellon University researchers were able to establish that people under psychological stress have higher than normal levels of proinflammatory cytokines in their nasal passages and systemically. These, not the virus, correlate with the symptoms of common colds. Put differently, common cold symptoms are a “side effect” of the inflammatory response that is triggered as part of the body’s effort to fight infection. The greater the body’s inflammatory response to the virus, the greater is the likelihood of experiencing the symptoms of a cold. Further when under stress, cells of the immune system are unable to respond to hormonal control, and consequently, produce levels of inflammation that promote disease.[1]
In brain-related diseases, a good example of this relationship was demonstrated in a very informative study of 300 mild-to-severe Alzheimer’s patients who were living on their own (not in assisted living.) First, with the assistance of their caregivers, they were assessed for a baseline level of cognitive function, tested for levels of a cytokine (pro-inflammatory) called Tumor Necrosis Factor alpha (TNF-a). They then recorded any new acute stressful systemic inflammatory event, such as an illness or physical trauma that occurred subsequent to the initial testing and retested cognitive function and the TNF-a levels at 2,4 and 6 months to compare to the baseline levels noted at the beginning of the study. The bottom line was that both acute and chronic systemic inflammation, as measured by increases in the pro-inflammatory TNF-a levels, correlated quite strongly with an increase in cognitive decline in the patients in the study.[2]
Up to 80% of patients with autoimmune diseases report uncommon emotional stress before the onset of their disease. Several studies also implicate stress in the exacerbation of autoimmune diseases and not only label stress as a participating factor but also a potential cause for autoimmune disease. Further, not only does stress cause disease, but the disease itself also causes significant stress in the patients, creating a vicious cycle. [3]
Stress Management
Where a Fire Marshall has matches, water and chemicals to start, manage and stop the controlled burning, our bodies are unfortunately not as easy to manage, as:
- They are made up of over 30 trillion cells and;
- A similar number of bacteria in our body, per a recent study out of the Weizmann Institute of Israel;
- Add to that the 20,000 or so genes that might be mutated plus;
- There are 50 hormones that can become irregular;
- All of which can affect one or more of our 78 organs.
In other words, battling our “physical fires” becomes far more complicated than fighting any forest fire we can imagine. Nonetheless, ADRCs are anti-inflammatory and modulate the immune system. They have immune cells that fight infections and have wound healing properties.
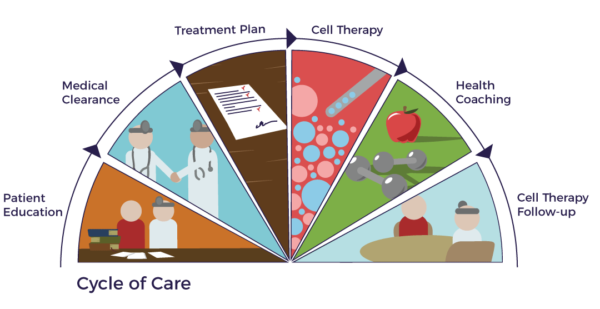 It makes common sense that managing excess stress and inflammation with sensible eating, exercise, a positive family/social environment and lifestyle improvements can enhance the benefits of AMBROSE Cell Therapy. By combining cell therapy with a well-controlled stress and inflammation level, it is like having the police, fire, emergency medical response, hospitals and social services departments all working in coordination to bring a riot under control, safely ensure the people in the community are well cared for and able to return to a normal life as soon as possible. All of these factors combine into the AMBROSE Cycle of Care.
It makes common sense that managing excess stress and inflammation with sensible eating, exercise, a positive family/social environment and lifestyle improvements can enhance the benefits of AMBROSE Cell Therapy. By combining cell therapy with a well-controlled stress and inflammation level, it is like having the police, fire, emergency medical response, hospitals and social services departments all working in coordination to bring a riot under control, safely ensure the people in the community are well cared for and able to return to a normal life as soon as possible. All of these factors combine into the AMBROSE Cycle of Care.
[1] S. Cohen et al Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk PNAS April 17, 2012 |vol. 109 no. 16 |5995–5999
[2] C. Holmes et al Systemic inflammation and disease progression in Alzheimer disease Neurology® 2009; 73:768–774
[3] L. Stojanovich, D. Marisavljevich Stress as a trigger of autoimmune disease Autoimmunity Reviews 7 (2008) 209–213
