AMBROSE Cell Therapy for Inflammatory Bowel Diseases (IBD)
Cell therapy for inflammatory bowel diseases harnesses the power of patients’ own adipose-derived stem and regenerative cells (ADRCs). This is a diverse population of cells that, through multiple activities, have the potential to help improve the symptoms, function and quality of life for patients living with conditions such as irritable bowel syndrome, ulcerative colitis, Celiac disease and Crohn’s disease.
These specialized cells are akin to having your own “biologic” fire, rescue and repair service. They wait quietly for a sign of trouble—inflammation—and home to that site to do their jobs. The scientists researching adult stem cell therapy for inflammatory bowel diseases now widely recognize that ADRCs reduce inflammation and rebalance the immune system in initiating the process of repair.[1] [2] [3] [4] [5]
Inflammatory bowel diseases involve a chronic inflammation of some part of the digestive tract and sometimes can be associated with inflammatory arthritis. IBD-associated arthritis of the spine begins with subtle low back pain, especially in younger persons, and morning stiffness. It gets worse with prolonged sitting or standing and improves with moderate activity. It is more common in CD than in UC and is independent of gastrointestinal symptoms.
Inflammatory-Immune Response
An inflammatory response can be triggered by a trauma, infection, environmental toxins, lifestyle choices (e.g. smoking), hereditary factors or a combination of those bad actors. This type of inflammation (acute) is essential for repairing the body, and is usually short-lived, disappearing once the healing process has taken place.
There is another type of lingering inflammatory response which becomes chronic, and affects the entire body, becoming systemic. Systemic inflammation is a common factor in diseases of aging—this covers a broad spectrum of severe, debilitating and, sometimes, life-threatening conditions.[6]
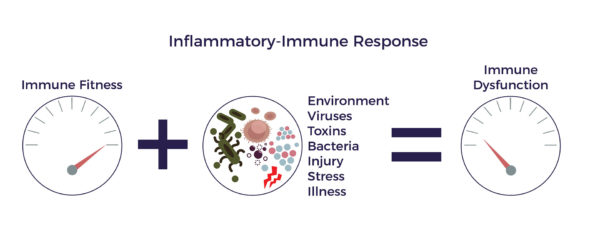
In the case of inflammatory bowel diseases, the chronic inflammation begins a vicious detrimental process. It recruits the immune system, which is there to fight infections and other disease processes, to assist healing. The cells in the immune system (immune cells) are there to guard the body. When they sense the enemy, they send out troops of pro-inflammatory molecules called “cytokines” to fight them off. When this process goes out of control, it is called an inflammatory-immune response. This response is tantamount to having a backseat driver who is chronically overreacting while “helping” you drive your car. It then leads to reduced blood flow (ischemia). Without good circulation, cells die off, scars form, tissues and organs degenerate. We call this the Spiral of Degeneration.
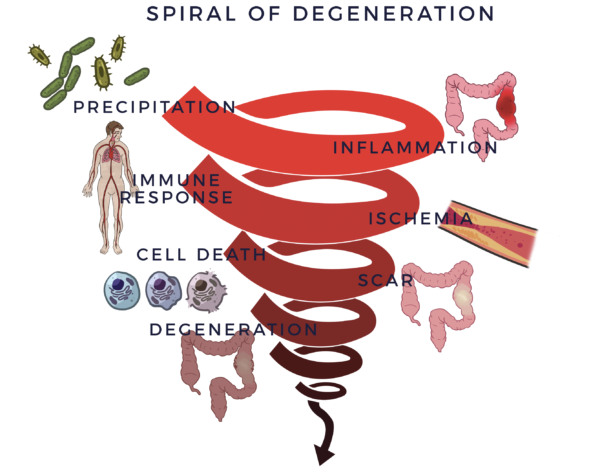
Inflammatory bowel diseases involve chronic systemic inflammation perpetuating the Spiral. Because of this, many patients with IBD have various forms of arthritis including but not limited to osteoarthritis, psoriatic arthritis and so forth. Systemic inflammation can sometimes manifest in IBD-associated lung, heart, kidney, brain or liver diseases or even cancers.
Process of Repair
Through a mechanism of cell-to cell communication known as the paracrine effect, ADRCs mobilize nearby cells to work more efficiently. They recruit the biologic fire, rescue and repair departments at the site—resident stem cells—to get back on the job and do their part.
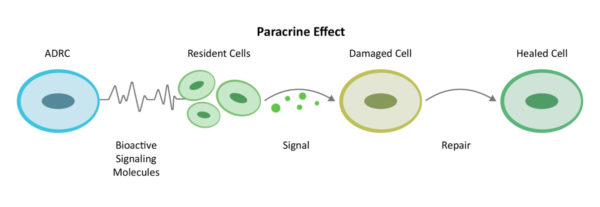
Recruiting additional “repairmen” at the site (resident stem cells) to get back on the job and do their part, ADRCs assemble an extended team and work first to decrease inflammation and the overactive immune responses. Once the backseat driving diminishes, they continue their work by increasing circulation with new blood vessel growth, preventing further cell death, addressing scar tissue and regenerating healthy tissue and nerves. This is how the body naturally heals, but if the insult from an acute or chronic condition is too great it needs help.
We call this the Process of Repair. It involves the multiple mechanisms of action that are needed to bring the systemic inflammation and immune response back to balance.
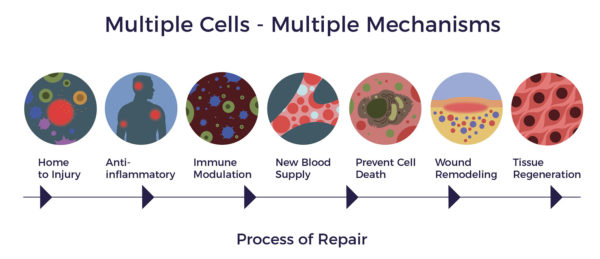
The process can extend to include the associated arthritic conditions as well as the organs affected by inflammatory bowel disease.
Stem cells have regenerative and modulatory properties on the immune system, which leads to reduction of inflammation and healing of affected intestinal tissue.[7] Stem cells infused by vein have been shown in human studies to significantly lessened disease Crohn’s Disease and Ulcerative Colitis, with one study reporting 68% of patients able to come off steroids after cell therapy. [8] [9] Longstanding remission has been achieved in some patients.[10]
Stem cells are well known for wound healing, and in human studies, stem cells have been shown to close fistulae associated with Crohn’s disease [11] [12] [13] [14] [15] as well as resolve inflammation in the fistula tract. [16] [17]
AMBROSE Cell Therapy for Inflammatory Bowel Diseases
AMBROSE Cell Therapy represents a minimally invasive option to improve symptoms, function and quality of life for patients with inflammatory bowel diseases. Personalized treatment plans are developed for each patient, taking into account each individual’s structural, biologic and medical status.
Please contact us for more information about treatment, candidacy and how to become a patient.
[1]JK Fraser PhD and S. Kesten MD Autologous Adipose Derived Regenerative Cells: A platform for therapeutic applications Advanced Wound Healing Surgical Technology International XXIX
[2] A Nguyen, A et al Stromal vascular fraction: A regenerative reality? Part 1: Current concepts and review of the literature Journal of Plastic, Reconstructive & Aesthetic Surgery (2016) 69, 170e179
[3] Guo et al Stromal vascular fraction: A regenerative reality? Part 2: Current concepts and review of the literature Journal of Plastic, Reconstructive & Aesthetic Surgery (2016) 69, 180e188
[4] F. De Francesco et al The role of adipose stem cells in inflammatory bowel disease: From biology to novel therapeutic strategies CANCER BIOLOGY & THERAPY 2016, VOL. 17, NO. 9, 889–898
[5] Qui et al Systematic review with meta-analysis: the efficacy and safety of stem cell therapy for Crohn’s disease Stem Cell Research & Therapy (2017) 8:136
[6] C. Franceschi and J. Campisi Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases J Gerontol A Biol Sci Med Sci 2014 June;69(S1): S4–S9
[7] Dave M, Mehta K, Luther J, Baruah A, Dietz AB, Faubion WA. Mesenchymal Stem Cell Therapy for Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. Inflamm Bowel Dis. 2015;21(11):2696–2707
[8] Lazebnik LB, Konopliannikov AG, Kniazev OV, et al. [Use of allogeneic mesenchymal stem cells in the treatment of intestinal inflammatory diseases] Ter Arkh. 2010;82:38–43
[9] Forbes GM, Sturm MJ, Leong RW, et al. A phase 2 study of allogeneic mesenchymal stromal cells for luminal Crohn’s disease refractory to biologic therapy. Clin Gastroenterol Hepatol. 2014;12:64–71
[10] Liang J, Zhang H, Wang D, et al. Allogeneic mesenchymal stem cell transplantation in seven patients with refractory inflammatory bowel disease. Gut. 2012;61:468–469
[11] Garcia-Olmo D, Garcia-Arranz M, Garcia LG, et al. Autologous stem cell transplantation for treatment of rectovaginal fistula in perianal Crohn’s disease: a new cell-based therapy. Int J Colorectal Dis. 2003;18:451–454
[12] Garcia-Olmo D, Garcia-Arranz M, Herreros D, et al. A phase I clinical trial of the treatment of Crohn’s fistula by adipose mesenchymal stem cell transplantation. Dis Colon Rectum. 2005;48:1416–1423
[13] Garcia-Olmo D, Herreros D, Pascual I, et al. Expanded adipose-derived stem cells for the treatment of complex perianal fistula: a phase II clinical trial. Dis Colon Rectum. 2009;52:79–86
[14] Cho YB, Lee WY, Park KJ, et al. Autologous adipose tissue-derived stem cells for the treatment of Crohn’s fistula: a phase I clinical study. Cell Transplant. 2013;22:279–285
[15] Lee WY, Park KJ, Cho YB, et al. Autologous adipose tissue-derived stem cells treatment demonstrated favorable and sustainable therapeutic effect for Crohn’s fistula. Stem Cells. 2013;31:2575–2581
[16] Ciccocioppo R, Bernardo ME, Sgarella A, et al. Autologous bone marrow-derived mesenchymal stromal cells in the treatment of fistulising Crohn’s disease. Gut. 2011;60:788–798
[17] de la Portilla F, Alba F, Garcia-Olmo D, et al. Expanded allogeneic adipose-derived stem cells (eASCs) for the treatment of complex perianal fistula in Crohn’s disease: results from a multicenter phase I/IIa clinical trial. Int J Colorectal Dis. 2013;28:313–323
