Can something be done for Covid Long-Haulers?
Can something be done for Covid Long-Haulers?
After living with severe long-Covid symptoms and pre-existing health conditions, Brian exercised his Right to Try AMBROSE Cell Therapy in November 2021. He says AMBROSE has had “a massive effect on my health and quality of life.” Brian adds, nine months out, “I am doing things I couldn’t do a month ago.”
Remarkably, Brian’s many benefits occurred despite ongoing business stress and the difficult loss of two family members.
Background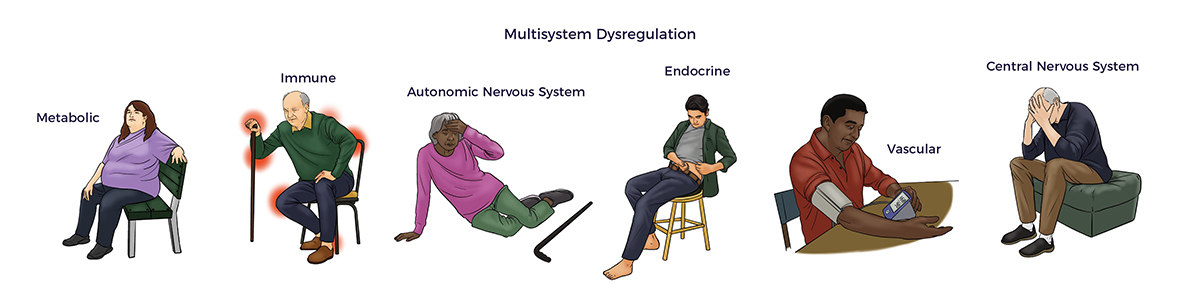 Since December 2019, SARS coronavirus 2 (SARS-CoV-2) has spread like wildfire across the globe. Unlike the seasonal flu or cold, COVID-19 can attack all body systems and multiple organs.
Since December 2019, SARS coronavirus 2 (SARS-CoV-2) has spread like wildfire across the globe. Unlike the seasonal flu or cold, COVID-19 can attack all body systems and multiple organs.
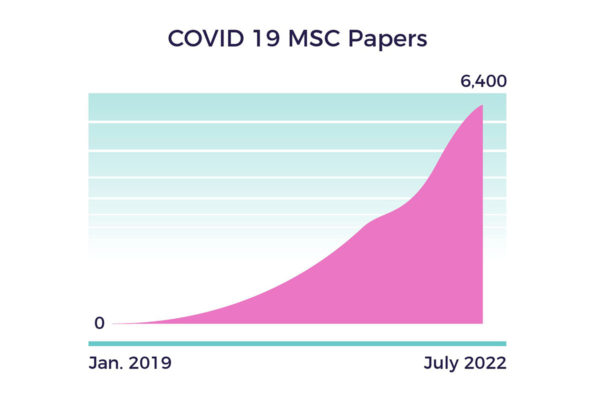
In response to the virus’ scorched earth capabilities, stem cell researchers worldwide have collaborated to improve outcomes for high-risk Covid patients and long-haulers. [1]
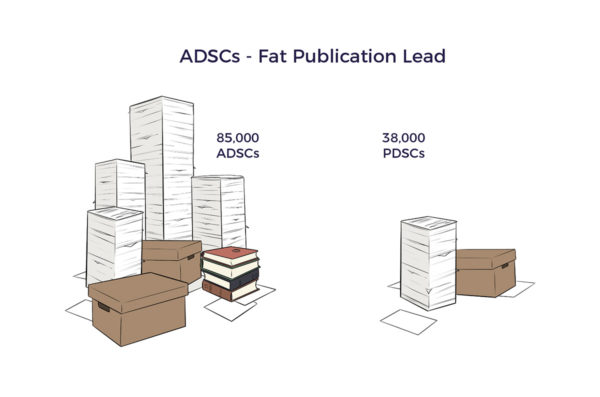
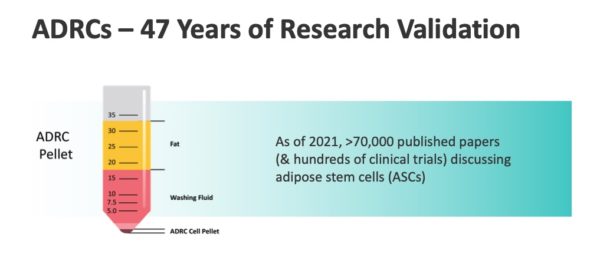
The researchers drew from over 200,000 published papers on Mesenchymal Stem Cells (MSCs). By July 2022, their urgency resulted in 6,400 articles or around 12 daily.
 The in-human MSC studies included Covid-induced:
The in-human MSC studies included Covid-induced:
- Acute respiratory distress syndrome (ARDS) [2]
- Multisystem inflammatory syndrome in children [3]
- Multi-organ disease, including sudden cardiac arrest [4]
- COVID-19 pneumonia in April 2020. [5]
Dr. Pietro Gentile and others focused their research on adipose-derived stem cells (ADSCs) and ADRCs. [6] [7] [8] [9]
Can ADRCs help Covid Long-Haulers?
 Most promising for Brian, his long-Covid symptoms intersected with those from hypermobility, concussions, renal failure, Lyme Disease, and post-chemo side effects.
Most promising for Brian, his long-Covid symptoms intersected with those from hypermobility, concussions, renal failure, Lyme Disease, and post-chemo side effects.
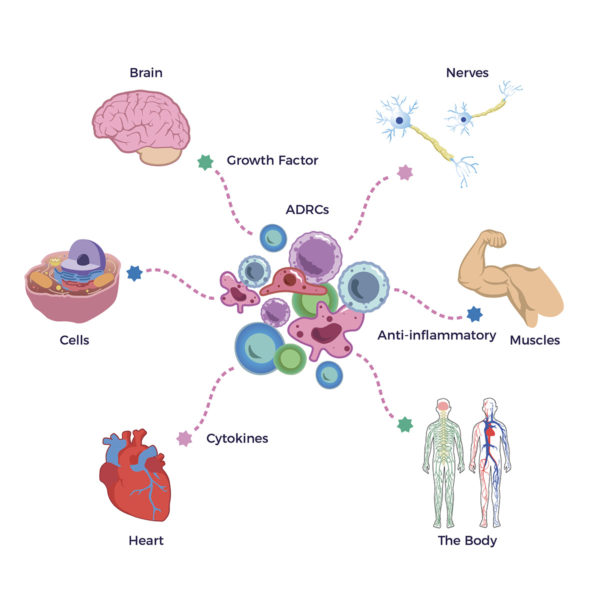
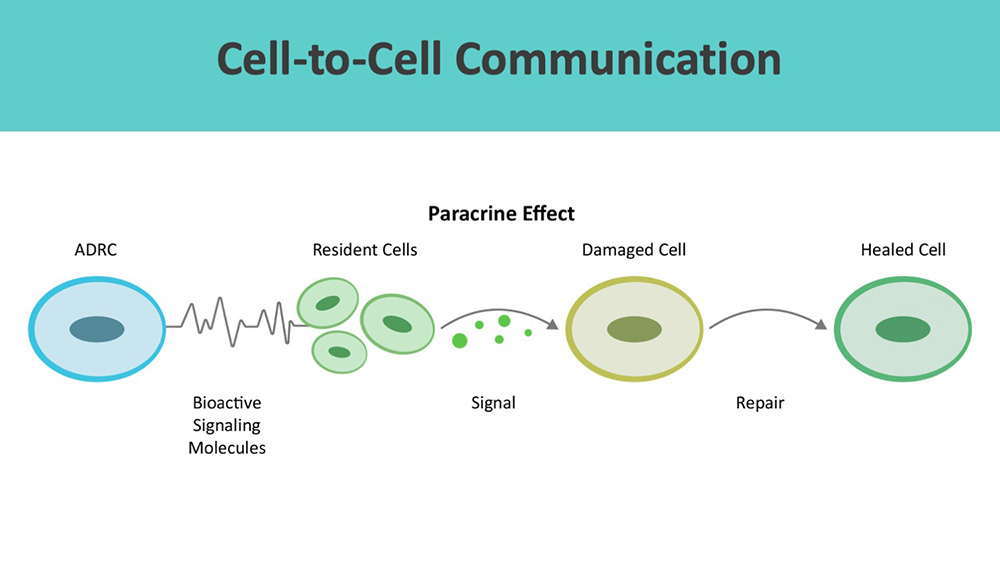
In response to one or more of these insults, our ADRCs secrete growth factors (GFs) and anti-inflammatory signaling proteins or cytokines essential to our brains, hearts, muscles, nerves, cells, and body health in general.
We share more on GFs and cytokines in Brian’s story that follows.
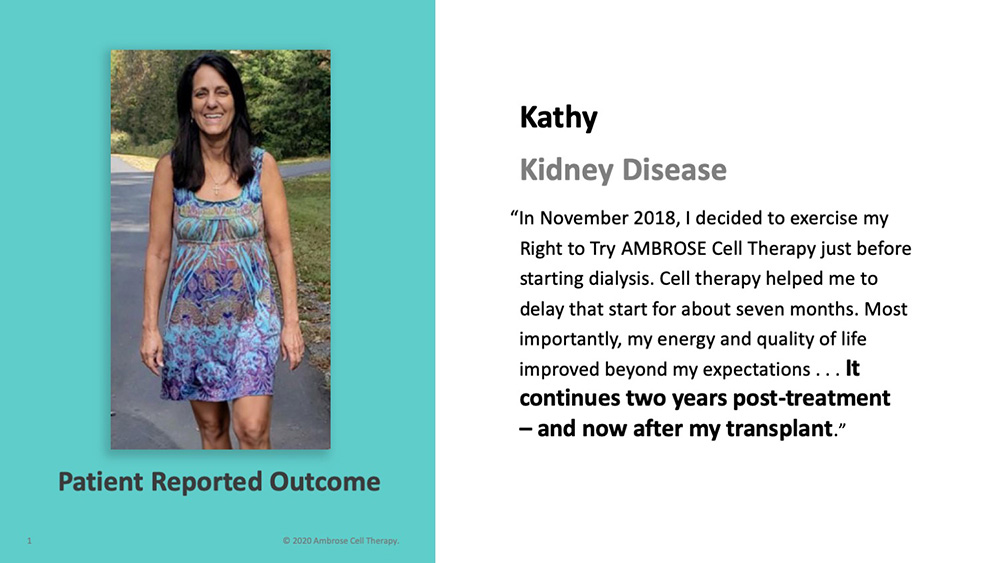
Ambrose patients Trish, Wouter, Kathy, and other patients with brain fog, fatigue, joint pain, and so on responded to ADRC-based therapy. Therefore, it made sense for Brian to try AMBROSE Cell Therapy.
Brian’s Story
In December 2020, Brian’s doctor admitted him to the Cedar-Sinai ICU with COVID-19, returning home as a Covid long-hauler after two weeks.
After an introductory call with CEO Matt Feshbach, AMBROSE provided an educational MD consult, overview articles, and peer-reviewed papers supporting the safety and potential effectiveness of the therapy for long-Covid and the other conditions affecting him. Brian said,” (Matt) answered my questions. I had sufficient understanding to move forward.”
Covid Long-Hauler Symptoms Brian experienced classic long-hauler symptoms: brain fog, chronic fatigue, and emotional volatility. As he summarized, “Most of 2021 was a lost year.”
Brian experienced classic long-hauler symptoms: brain fog, chronic fatigue, and emotional volatility. As he summarized, “Most of 2021 was a lost year.”
He started to notice benefits shortly after his AMBROSE treatment. “After about a month, I saw a massive improvement in my mental clarity and energy. Business associates said they noticed the difference too. I didn’t realize how bad the fatigue was until I regained my strength.”
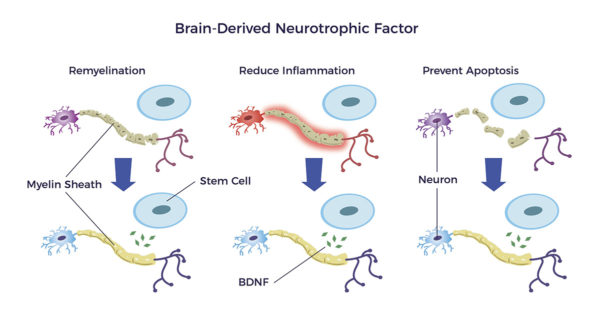
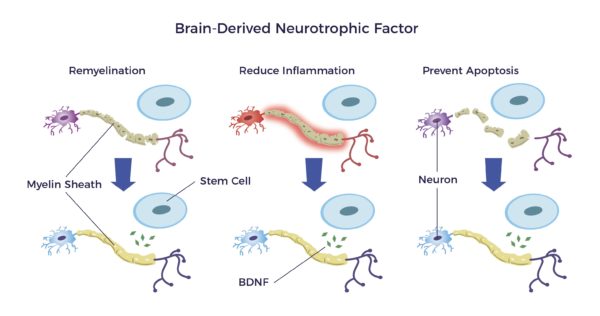
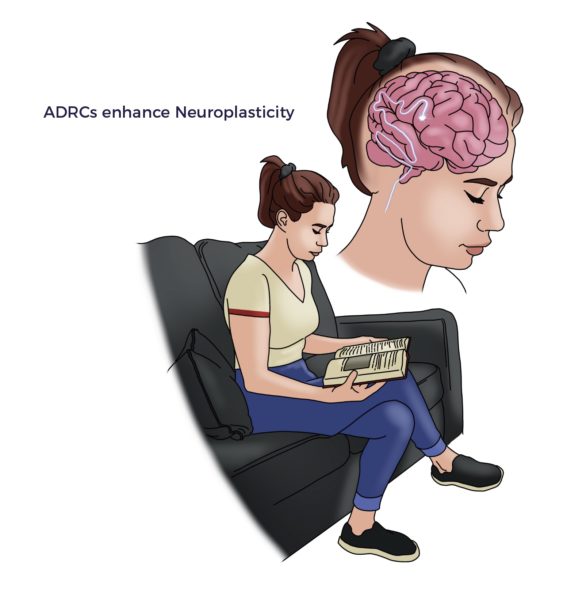
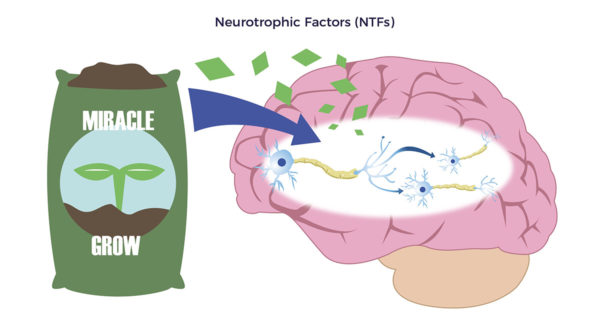 Supporting Brian’s statements, ADRCs release “Neurotrophic factors (NTFs),” Neuro relating to nerve and trophic, from Ancient Greek trophikós, meaning” of food or nourishment.” NTFs, through multiple mechanisms, reduce neuroinflammation and stimulate the development of new brain cells, brain cell connections, and nerves. [10] [11]
Supporting Brian’s statements, ADRCs release “Neurotrophic factors (NTFs),” Neuro relating to nerve and trophic, from Ancient Greek trophikós, meaning” of food or nourishment.” NTFs, through multiple mechanisms, reduce neuroinflammation and stimulate the development of new brain cells, brain cell connections, and nerves. [10] [11]
Just as fertilizers keep plants healthy and growing, neurotrophic factors work like Miracle Grow for the brain.
Brian’s restored energy and mental clarity make sense in light of the above.
Vasculitis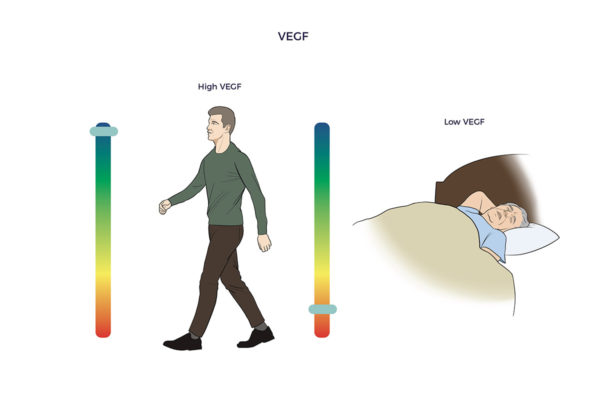 Covid left Brian with debilitating inflamed blood vessels and swelling in both legs, or vasculitis, an autoimmune condition. He also complained of constant numbness and tingling in both legs (neuropathy). The right leg was worse than the left.
Covid left Brian with debilitating inflamed blood vessels and swelling in both legs, or vasculitis, an autoimmune condition. He also complained of constant numbness and tingling in both legs (neuropathy). The right leg was worse than the left.
“My vasculitis and neuropathy went away shortly following the treatment.”
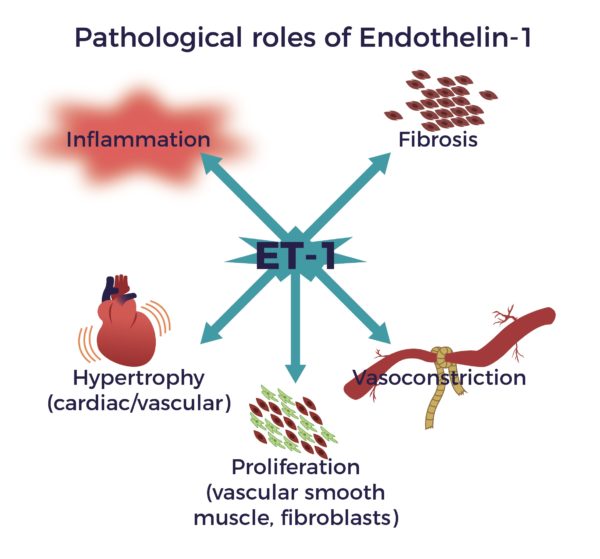
In addition to the NTFs, ADRCs secrete Vascular Endothelial Growth Factor (VEGF). VEGF improves circulation, reduces inflammation, and stimulates the growth of new blood vessels.
Here again, it makes sense that Brian’s swollen blood vessels and nerves calmed down. And an abundance of literature supports Brian’s subjective experience. [12] [13]
And back to Brian’s brain: VEGF reduces neuroinflammation and improves blood flow in the brain. In contrast, neuroinflammation and lack of blood flow in the brain cause chronic fatigue, brain fog, and memory issues. [14] [15]
Pre-Existing Conditions
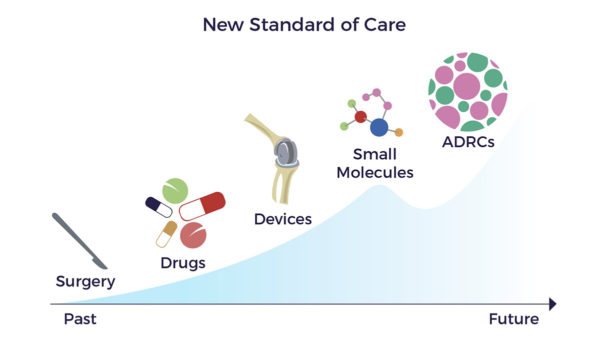
Brian entered the hospital with a galaxy of pre-existing conditions that had failed to improve with surgeries, drugs, and devices.
Before the pandemic, Brian lived with:
- Obesity
- Arthritis in his lower back, shoulders, hips, and knees
- Asthma
- Fractured ribs
- Osteopenia (an early stage of osteoporosis) and
- A mildly enlarged heart and shortness of breath
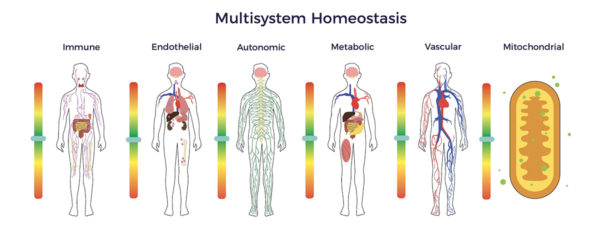
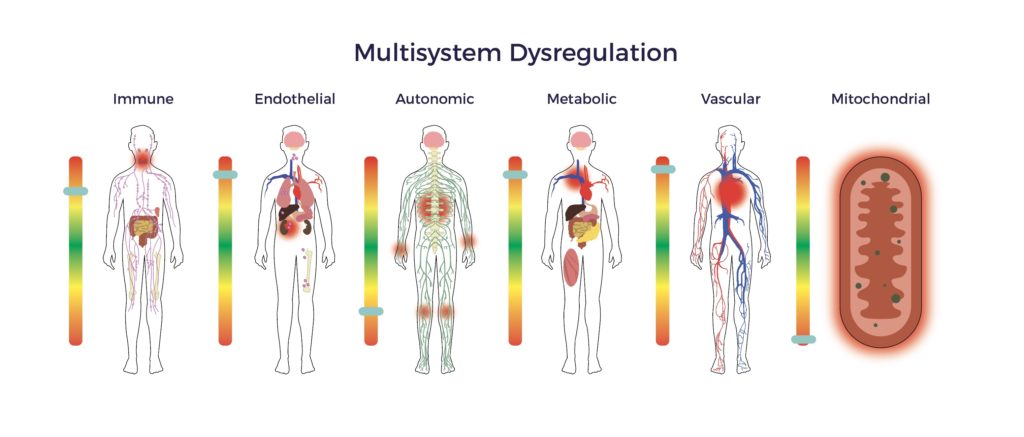
In summary, Brian suffered from multisystem dysregulation.
His medications included Prednisone 30-mg daily, Singulair, Symbicort, and Spiriva for Asthma. Ambien for sleep.
Can ADRCs help Covid long-haulers with pre-existing conditions?
In 2016 The California Institute of Regenerative Medicine (CIRM) contributed funding to two review papers that supported ADRC-based treatment for Brian’s chronic illnesses. Further, preeminent researchers from Tulane University and other respected research institutions have continued the growing support for ADRCs’ potential to treat multiple diseases. [16] [17] [18]
Obesity
Brian has struggled with his weight since a young age. “I have probably lost 300 lbs. throughout my life. I tried bariatric surgery in 2007 but gained the weight back.”
“Since my treatment, I have dropped about 50 lbs. and have maintained my weight within a lower range with a less restrictive diet for the first time.”
In 1994, super-sleuth Jeffrey M. Friedman of Rockefeller University established fat as an endocrine organ. In simple terms, he discovered adipose cells secrete hormones that regulate weight gain. His insight explains Brian’s improved metabolism and fat burning following his cell therapy treatment. [19] [20]
Wear, Tear, and Trauma
Brian played football in high school, resulting in some head traumas. He was involved in several major motor vehicle accidents in his early 20s. He went unconscious twice. “They took me to the hospital several times; it was pretty bad.”
Football, basketball, baseball, skiing, and excess weight was not kind to Brian’s joints either.
- Three right-knee operations failed, leaving both knees painful.
- He experienced degenerative arthritis in his shoulders.
- His right and left hips were arthritic as well.
Steroid injections in the affected joints failed to give Brian relief. He tried bone-marrow stem cell injections for his shoulders, but that “didn’t work at all.”
Ambrose’s interventional pain specialist developed a personalized treatment plan based on a Master Protocol. He delivered 22 injections of PRP-enriched micronized fat into Brian’s painful joints.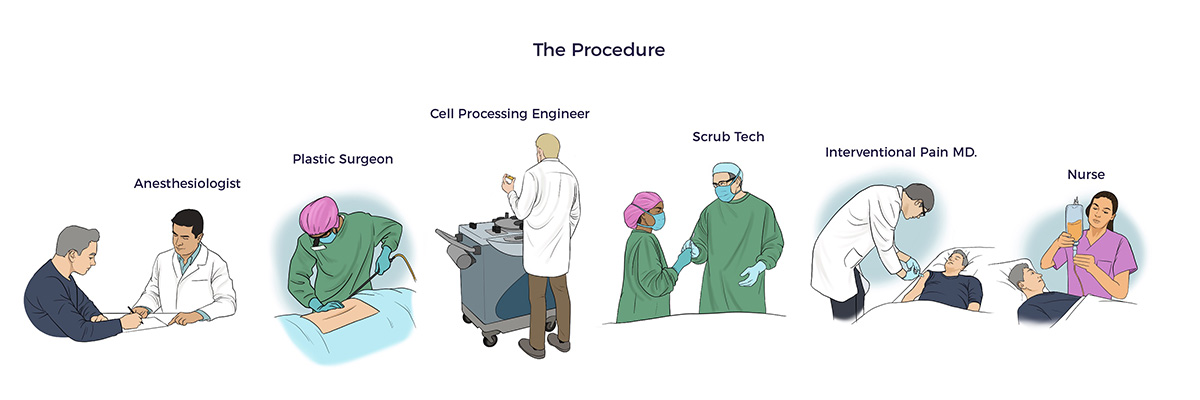
A month out, his PT said, “Brian’s weight-bearing tolerance and conditioning are improving. He’s doing great.”
Eight months out, Brian shared, “My shoulder, hips, and knees feel good. My back is fine.”
Asthma
Brian developed asthma in his 40s after spending a month in China on business. Before his stem cell treatment, he used three inhalers and took 30 mg of prednisone daily.
Nine months after Brian’s AMBROSE treatment, he says, “I have lowered my daily prednisone dose to 10 mg and occasionally miss taking it without an asthma flare. I significantly reduced my use of inhalers, too.”
Fractured Ribs
An asthma-induced coughing attack fractured four ribs on March 1, 2018. After reviewing Brian’s x-rays, his orthopedist told him he could not repair the ribs. Additionally, Brian had an underlying diagnosis of osteopenia, a condition involving reduced bone mass.
Studies showed that ADRCs stimulate bone healing. [21]
The Ambrose physician injected the fractured ribs. Several months later, Brian reported, “My ribs feel like they healed. That is impressive” To be clear, he still experiences mild discomfort, “but nothing like it was before.”
Mildly Enlarged Heart
A 2018 cardiac workup revealed Brian had a mildly enlarged heart and shortness of breath.
His cardiologist and PT agree the shortness of breath is no longer evident.
The PRECISE cardiac cell therapy study demonstrated significant improvements in endurance, thus supporting Brian’s doctor’s observations. [22] A new cardiac workup is in order.
Multisystem Balance Restored
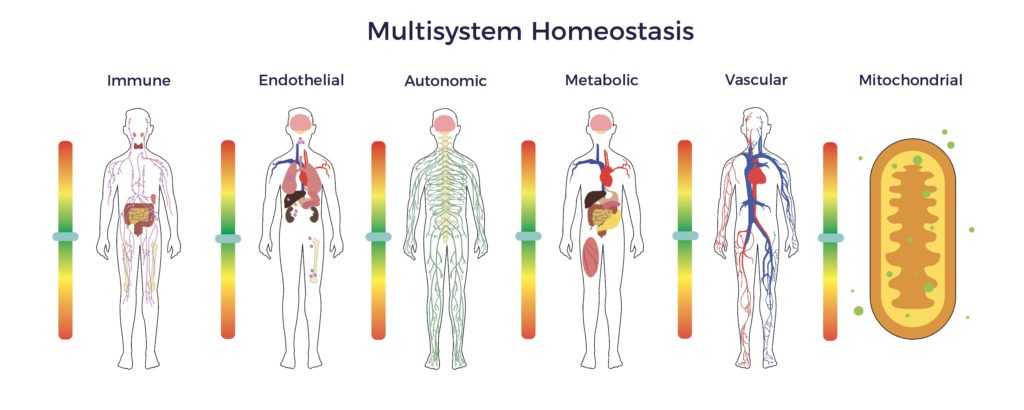
Brian’s patient-reported outcome demonstrates the potential to restore multisystem homeostasis (balance) by utilizing his ADRCs.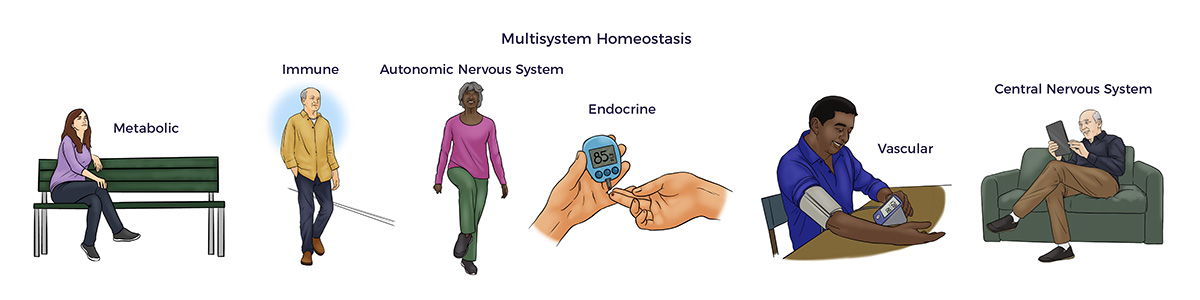
 Recommending AMBROSE to Family and Friends
Recommending AMBROSE to Family and Friends
“I have recommended Ambrose to my mother and best friend. It makes sense for them to try it too. Both have arthritic joints, back pain, and other medical issues.”
[1] Yasamineh et al. Spotlight on therapeutic efficiency of mesenchymal stem cells in viral infections with a focus on COVID-19 Stem Cell Research & Therapy (2022) 13:257
[2] Wick K et al. Mesenchymal stromal cells reduce evidence of lung injury in patients with ARDS JCI Insight 2021;6(11):e148983
[3] Ross Eckard A, Borow KM, Mack EH, Burke E, Atz AM. Remestemcel-L therapy for
COVID-19-associated multisystem inflammatory syndrome in children. Pediatrics. 2021
[4] Yilmaz R et al. Mesenchymal stem cells treatment in COVID-19 patient with multi-organ involvement Bratisl Med J 2020; 121 (12) 847-852
[5] Zeng et al. Transplantation of ACE2- Mesenchymal Stem Cells Improves the Outcome of Patients with COVID-19 Pneumonia Aging & Disease Volume 11 Number 2; 216-228, April 2020
[6] Stromal Vascular Fraction or SVF is the generic term for clinical grade adipose-derived regenerative cells.
[7] Pietro Gentile, Aris Sterodimas. Adipose Stem Cells (ASCs) and Stromal Vascular Fraction (SVF) as a Potential Therapy in Combating (COVID-19)-Disease. Aging and disease. 2020, 11(3): 465-469
[8] Alexander RW. (2020) Overview of COVID-19 Lung Damage Clinical Trial Using Cellular
Stromal Vascular Fraction (cSVF) and Functional Respiratory Imaging (FRI) Analysis of Pulmonary Injury
& Post-Viral (SARS-CoV-2) Adult Respiratory Distress Syndrome (ARDS). Stem Cell Res. 1(1)-1-19.
[9] Sanchez-Guijo F et al. Adipose-derived mesenchymal stromal cells for the treatment of patients with severe SARS-CoV-2 pneumonia requiring mechanical ventilation. A proof of concept study EClinical Medicine 000 (2020) 100454
[10] S. Seigo et al, Uncultured adipose-derived regenerative cells promote peripheral nerve regeneration, Journal of Orthopaedic Science, Volume 18, Issue 1,2013, Pages 145-151
[11] Xu et al Brain-derived neurotrophic factor reduces inflammation and hippocampal apoptosis in experimental Streptococcus pneumoniae meningitis Journal of Neuroinflammation (2017) 14:156
[12] Liao L. Mesenchymal stem cell and hematopoietic stem cell transplantation for vasculitis. Vasc Invest Ther 2020; 3:88‐93.
[13] Jahangir S et al. New advanced therapy medicinal products in treatment of autoimmune diseases Editor(s): Nima Rezaei, In Translational Immunology, Translational Autoimmunity, Academic Press, Volume 2, 2022, Pages 319 359,
[14] Skok M. Mesenchymal stem cells as a potential therapeutic tool to cure cognitive impairment caused by neuroinflammation. World J Stem Cells 2021; 13(8): 1072-1083
[15] J Rosenstein, J Krum & C Ruhrberg VEGF in the nervous system Organogenesis 6:2, 107-114; April/May/June 2010; © 2010 Landes Bioscience
[16] Nguyen A et al. Stromal vascular fraction: A regenerative reality? Part 1: Current concepts and review of the literature Journal of Plastic, Reconstructive & Aesthetic Surgery (2016) 69, 170e179
[17] Guo J et al. Stromal vascular fraction: A regenerative reality? Part 2: Mechanisms of regenerative action Journal of Plastic, Reconstructive & Aesthetic Surgery (2016) 69, 180e188
[18] Al-Ghadban S, Artiles M, Bunnell BA. Adipose Stem Cells in Regenerative Medicine: Looking Forward. Front Bioeng Biotechnol. 2022; 9:837464. Published 2022 Jan 13.
[19] Zhang, Y; Proenca, R; Maffei, M; Barone, M; Leopold, L; Friedman, JM (December 1994). “Positional cloning of the mouse obese gene and its human homologue”. Nature. 1994 (372): 425–432
[20] Zuccarini, M et al Adipose Stromal/Stem Cell-Derived Extracellular Vesicles: Potential Next-Generation Anti-Obesity Agents. Int. J. Mol. Sci.
2022, 23, 1543.
[21] Saxer F et al. Implantation of Stromal Vascular Fraction Progenitors At Bone Fracture Sites: From A Rat Model To A First-In-Man Study STEM CELLS 2016; 00:00-00
[22] Perin E et al., Adipose-derived regenerative cells in patients with ischemic cardiomyopathy: The PRECISE Trial Am Heart J 2014;168:88-95.e2.








 By 86, Parkinson’s had disabled, depressed, and hurt Mary. Tremors prevented her from using a fork and knife.
By 86, Parkinson’s had disabled, depressed, and hurt Mary. Tremors prevented her from using a fork and knife.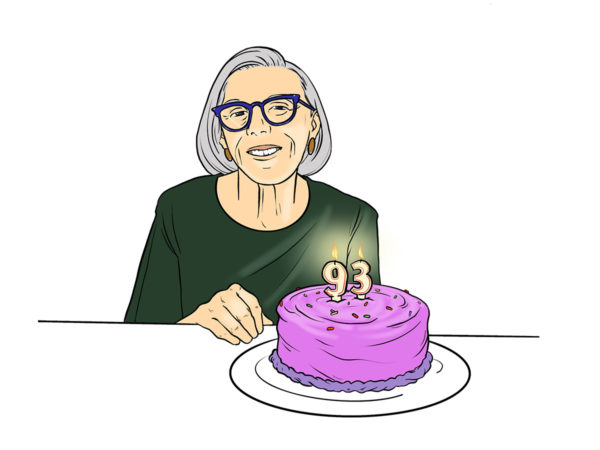 In October 2014, Ambrose’s predecessor group treated Mary with a novel ADRC-based protocol, which sparked her Comeback to the Future. Seven years after that single treatment, Mary celebrated her 93rd birthday with friends.
In October 2014, Ambrose’s predecessor group treated Mary with a novel ADRC-based protocol, which sparked her Comeback to the Future. Seven years after that single treatment, Mary celebrated her 93rd birthday with friends.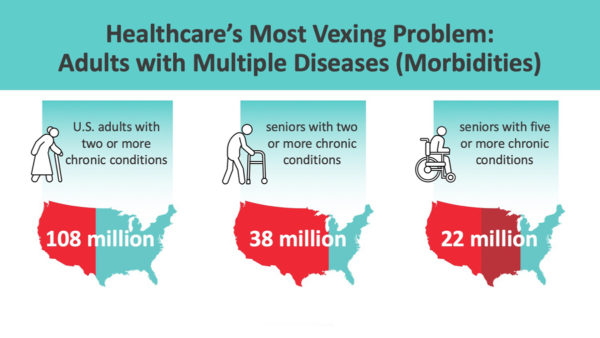 As we age, the situation becomes dire: The average senior sees seven doctors and takes seven meds per year.
As we age, the situation becomes dire: The average senior sees seven doctors and takes seven meds per year.
 In the mid-1960s,
In the mid-1960s, 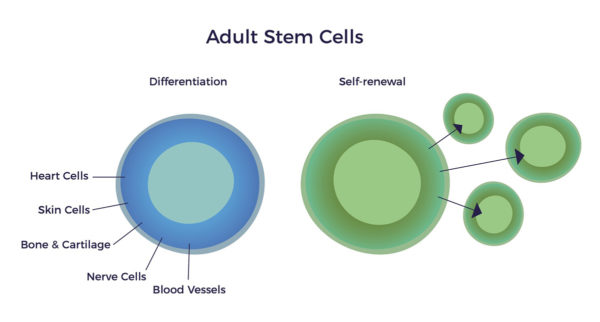
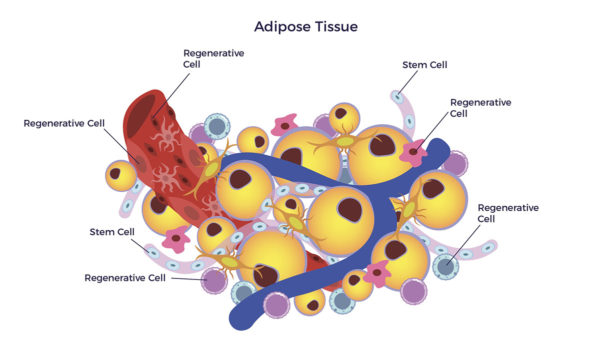
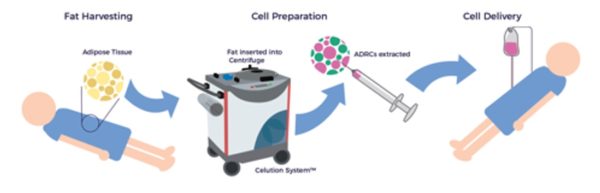
 Ten years later, UCLA researchers Patricia Zuk et al. discovered the most accessible, abundant, and potent source of MSCs: Adipose Tissue. Zuk’s group bridged the gap between the age-old science of physiology and the new-age medicine of ADRCs.
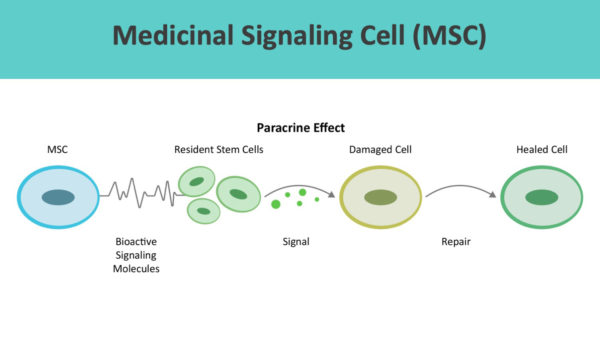
Ten years later, UCLA researchers Patricia Zuk et al. discovered the most accessible, abundant, and potent source of MSCs: Adipose Tissue. Zuk’s group bridged the gap between the age-old science of physiology and the new-age medicine of ADRCs. ADRCs contain DNA in each cell’s nucleus. Thus, they adhere to Caplan’s Medicinal Signaling Cell framework.
ADRCs contain DNA in each cell’s nucleus. Thus, they adhere to Caplan’s Medicinal Signaling Cell framework.
 In 2006, Dr. William Langston, the Michael J. Fox Foundation’s first Chief Science Officer, published The Parkinson’s Complex: Parkinsonism Is Just the Tip of the Iceberg.
In 2006, Dr. William Langston, the Michael J. Fox Foundation’s first Chief Science Officer, published The Parkinson’s Complex: Parkinsonism Is Just the Tip of the Iceberg.  Succinctly, as we age, our cells, tissues, organs, and systems lose harmony.
Succinctly, as we age, our cells, tissues, organs, and systems lose harmony.  In scientific terms, her restorative cells secreted hundreds of healing, or trophic factors, that signaled the resident cells to resume playing according to her musical score.
In scientific terms, her restorative cells secreted hundreds of healing, or trophic factors, that signaled the resident cells to resume playing according to her musical score. In the real world, Mary’s mood, energy, motor control, balance, and pain score remain improved for more than seven years.
In the real world, Mary’s mood, energy, motor control, balance, and pain score remain improved for more than seven years.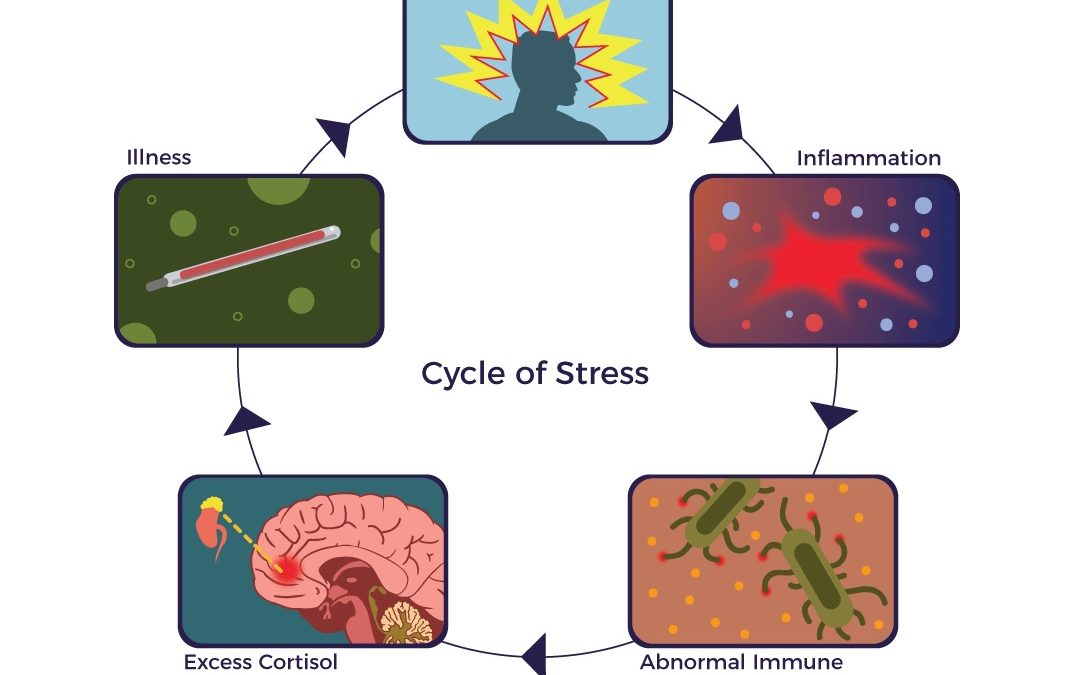

 What causes a flare?
What causes a flare?
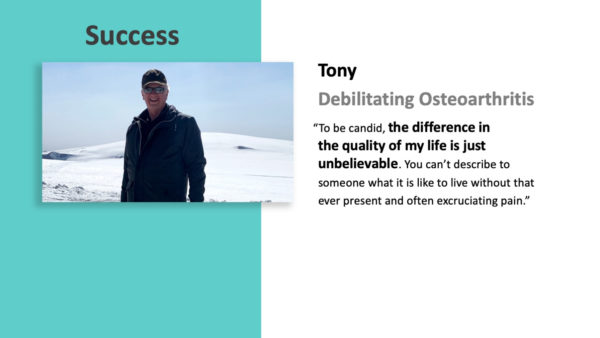
 Apparently, Tony didn’t know
Apparently, Tony didn’t know 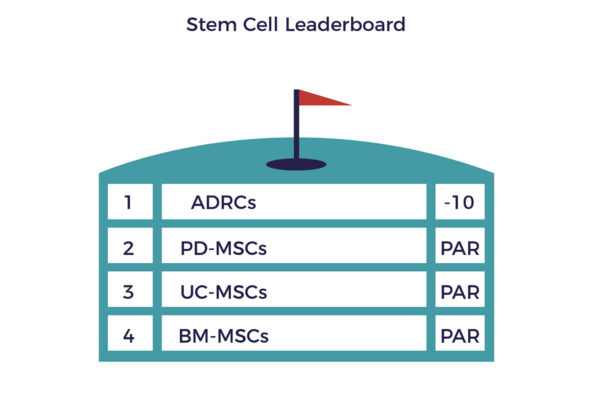 Note, Jack said “helped me” – stem cells are the fertilizer – physical therapy, appropriate exercise, and a healthy lifestyle are the gardeners that restore health.
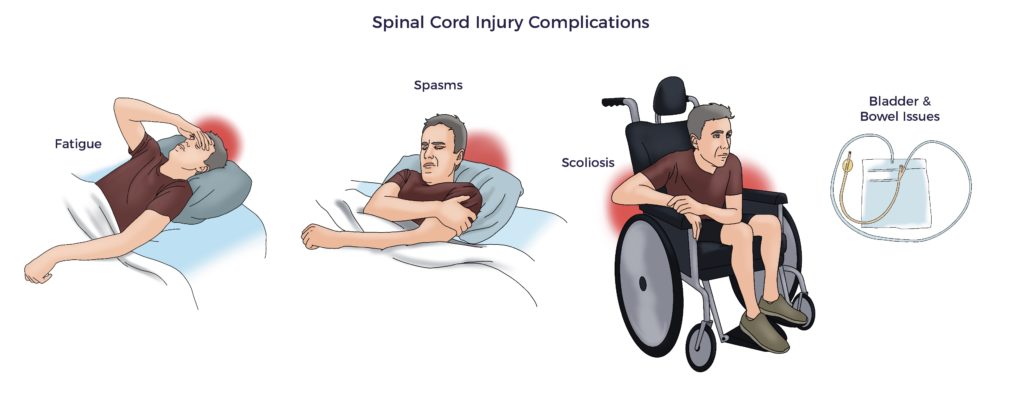
Note, Jack said “helped me” – stem cells are the fertilizer – physical therapy, appropriate exercise, and a healthy lifestyle are the gardeners that restore health.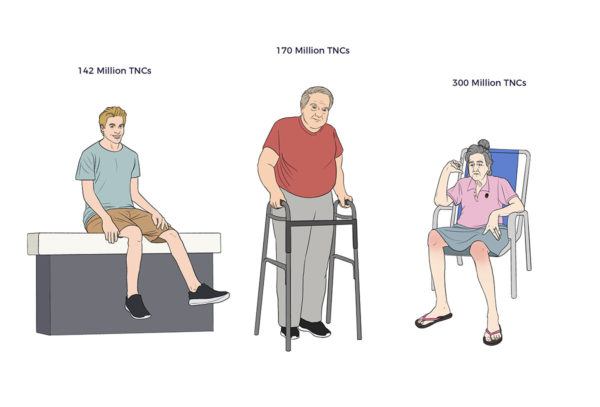 On the other side of the coin, a 15-year-old spinal cord injury patient’s yield was right up there with Bob. Six months post-cell therapy and more than one year after his catastrophic injury, the young man regained bilateral motor control of his hip flexors and quads. Standard of Care SCI patients plateau at about 12-months – remarkably, this young man’s path is accelerating.
On the other side of the coin, a 15-year-old spinal cord injury patient’s yield was right up there with Bob. Six months post-cell therapy and more than one year after his catastrophic injury, the young man regained bilateral motor control of his hip flexors and quads. Standard of Care SCI patients plateau at about 12-months – remarkably, this young man’s path is accelerating.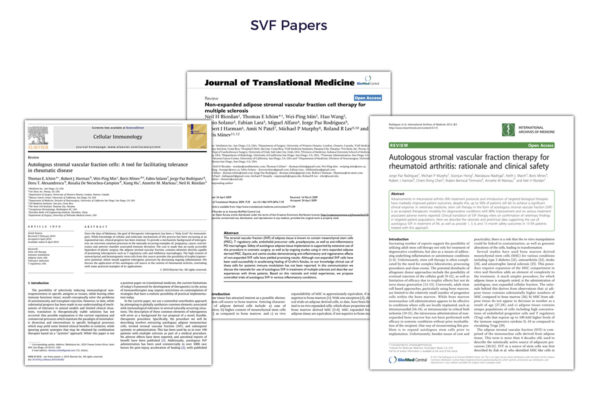 Recent research clarifies that donor stem cells are “immune-evasive, not immune-privileged,” counter to the proponents of allogeneic cell therapy.
Recent research clarifies that donor stem cells are “immune-evasive, not immune-privileged,” counter to the proponents of allogeneic cell therapy.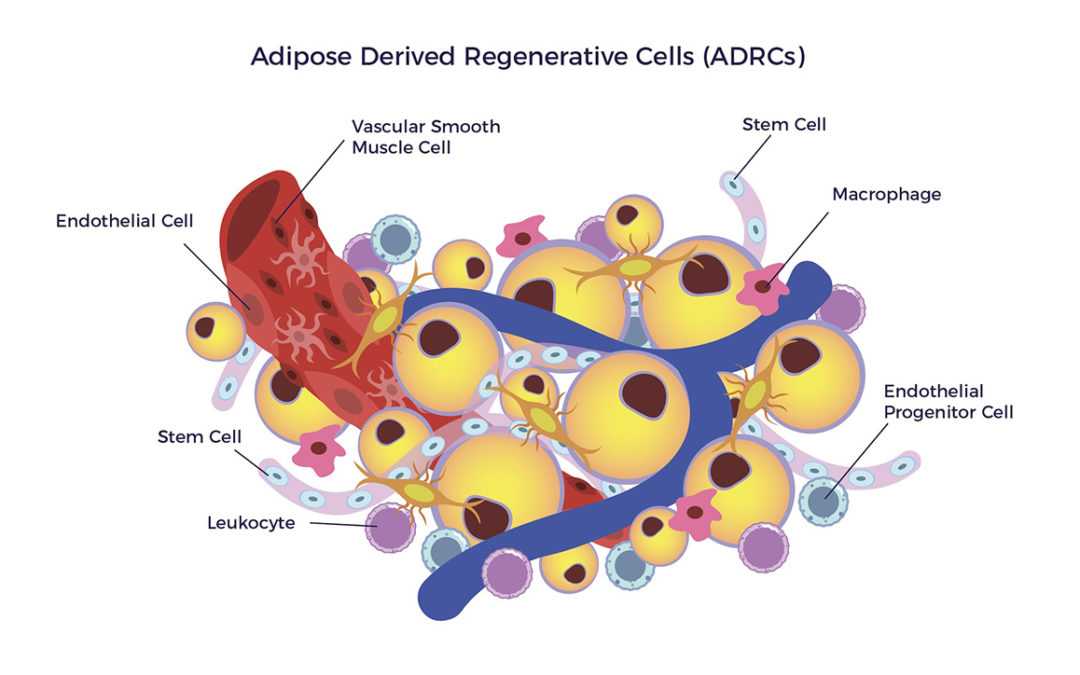
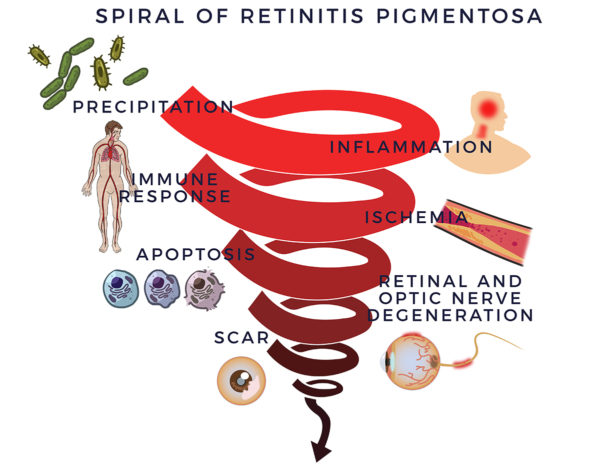 In 1857, Dr. Donders identified a group of incurable eye disorders he named retinitis pigmentosa (RP). But it was not as simple as that: Subsequently, researchers discovered over 100 genes that can contain mutations leading to retinitis pigmentosa. But genetic abnormalities do not clarify everything; half of RP cases lack previous family history and explanation.
In 1857, Dr. Donders identified a group of incurable eye disorders he named retinitis pigmentosa (RP). But it was not as simple as that: Subsequently, researchers discovered over 100 genes that can contain mutations leading to retinitis pigmentosa. But genetic abnormalities do not clarify everything; half of RP cases lack previous family history and explanation.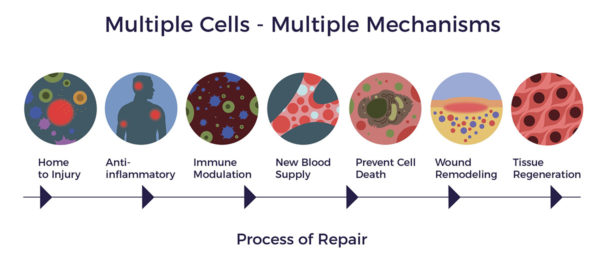
 Drug and gene therapy developers continue to pursue the failed “one molecule or gene for one disease model” for RP. This minimalist approach has not produced a drug or gene therapy that changes disease progression or improves patients’ best-corrected visual acuity (BCVA).
Drug and gene therapy developers continue to pursue the failed “one molecule or gene for one disease model” for RP. This minimalist approach has not produced a drug or gene therapy that changes disease progression or improves patients’ best-corrected visual acuity (BCVA).

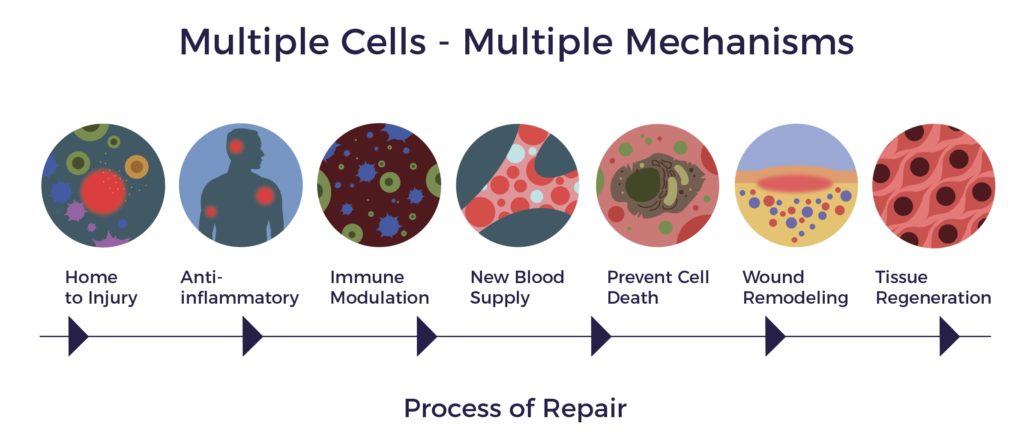
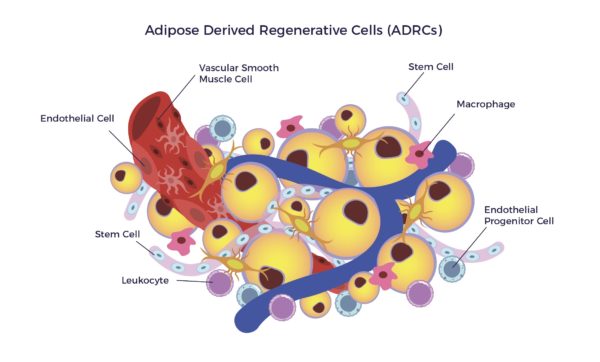
 ADRCs are a heterogeneous population of cells, including mesenchymal stem cells, other progenitor cells, fibroblasts, T-regulatory cells, and macrophages. The mix includes a high percentage of endothelial cells, endothelial progenitor cells, macrophages, and leukocytes.
ADRCs are a heterogeneous population of cells, including mesenchymal stem cells, other progenitor cells, fibroblasts, T-regulatory cells, and macrophages. The mix includes a high percentage of endothelial cells, endothelial progenitor cells, macrophages, and leukocytes.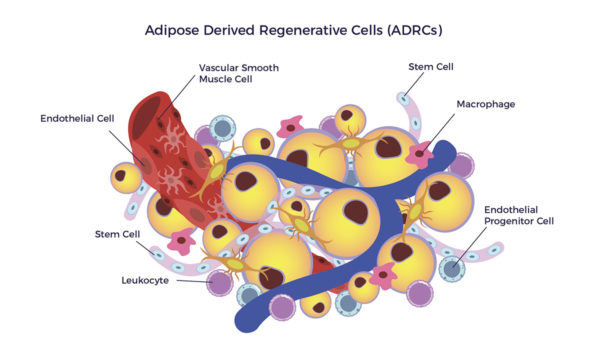 After homing to an inflammatory signal, the ADRC-secretome releases hundreds of cytokines and growth factors to the diseased microenvironment. The endogenous cells send signals back to the ADRCs.
After homing to an inflammatory signal, the ADRC-secretome releases hundreds of cytokines and growth factors to the diseased microenvironment. The endogenous cells send signals back to the ADRCs.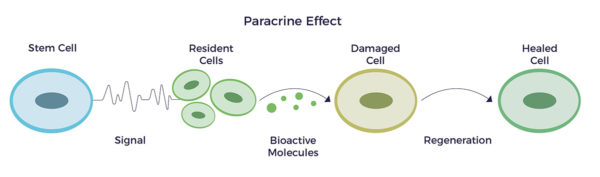
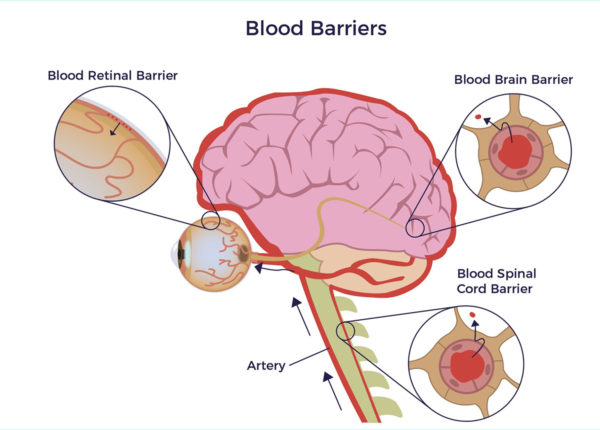 Permeating the Blood-Retinal-Barrier
Permeating the Blood-Retinal-Barrier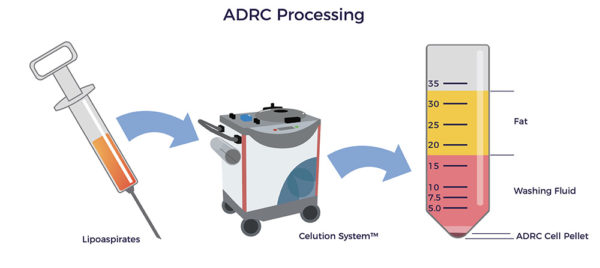 More than 40 countries have approved Celution for clinical use, including the United Kingdom, the European Union, Japan, South Korea, and New Zealand. Additionally, FDA has approved Celution for nine clinical trials.
More than 40 countries have approved Celution for clinical use, including the United Kingdom, the European Union, Japan, South Korea, and New Zealand. Additionally, FDA has approved Celution for nine clinical trials.
 But the average senior sees seven doctors and takes seven meds per year. Thus, we all know someone – or are that someone – who lives with a poor quality of life.
But the average senior sees seven doctors and takes seven meds per year. Thus, we all know someone – or are that someone – who lives with a poor quality of life. Self-proclaimed biohacking broscientists are on the other end of the spectrum.
Self-proclaimed biohacking broscientists are on the other end of the spectrum. If something might just help your health – no proof required- one of the broscientists will sell or promote it. In doing so, they claim their products, equipment, books, podcasts, and psychedelic drugs are the solution to everything from chronic disease to healthy aging.
If something might just help your health – no proof required- one of the broscientists will sell or promote it. In doing so, they claim their products, equipment, books, podcasts, and psychedelic drugs are the solution to everything from chronic disease to healthy aging.
 Like big pharma, biohacking is big business. If we stacked on top of one another all the equipment, products, supplements, coffee, food, books, course materials, franchise documents, blog posts, and transcripts the big three market, it would be the height of a 10-story super-store.
Like big pharma, biohacking is big business. If we stacked on top of one another all the equipment, products, supplements, coffee, food, books, course materials, franchise documents, blog posts, and transcripts the big three market, it would be the height of a 10-story super-store. The polar opposites are the stars of the back-to-basics formula. They are everyday folks who enjoy life into their 80s, 90s, and 100s with intact memories, healthy hearts, and rich social lives.
The polar opposites are the stars of the back-to-basics formula. They are everyday folks who enjoy life into their 80s, 90s, and 100s with intact memories, healthy hearts, and rich social lives. On a personal basis, the pillars of the Power of Simplicity encompass the future of healthy, happy, and dignified aging. And you can splurge on them without having to spend any money at the Biohacking Superstore.
On a personal basis, the pillars of the Power of Simplicity encompass the future of healthy, happy, and dignified aging. And you can splurge on them without having to spend any money at the Biohacking Superstore.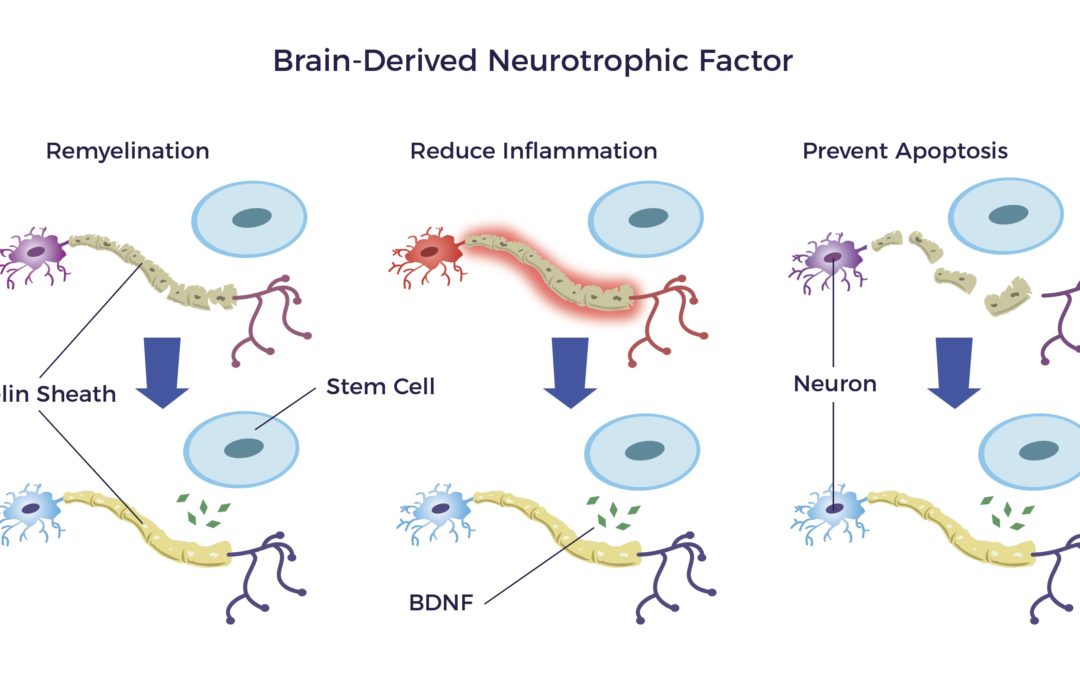


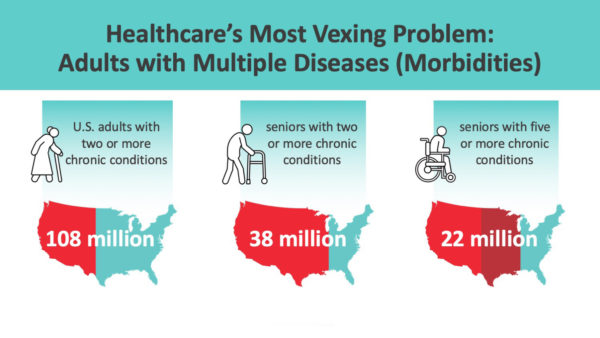


 Alexander’s feat is trivial compared to untying the intricate web of tangles involved in caring for no-option patients. This dilemma is even more complicated than it may first appear.
Alexander’s feat is trivial compared to untying the intricate web of tangles involved in caring for no-option patients. This dilemma is even more complicated than it may first appear.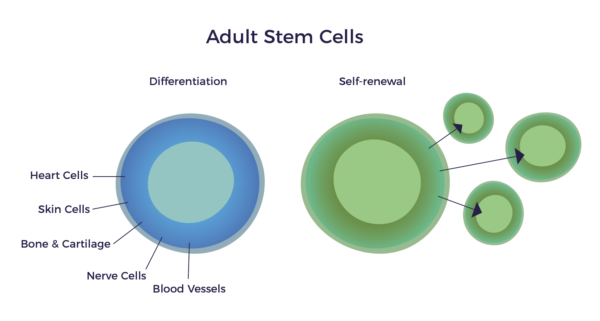
 As a testament to Dr. Caplan’s vision and research, according to a
As a testament to Dr. Caplan’s vision and research, according to a 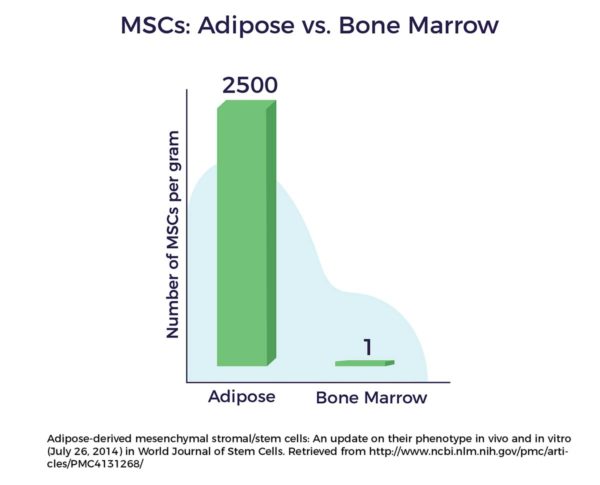
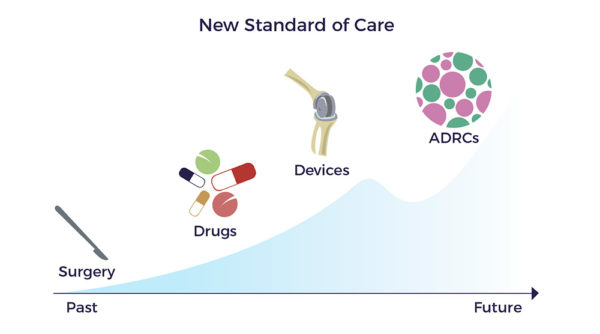
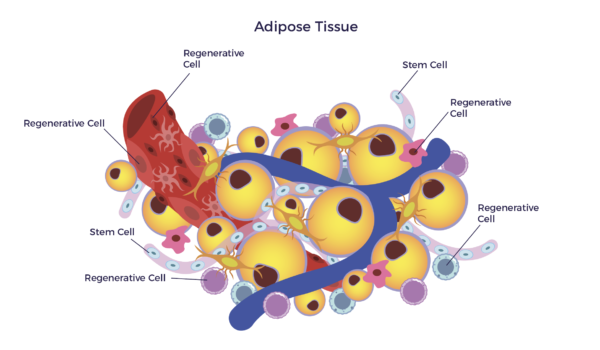 In other words, there is a mixed population of stem cells and other regenerative cells in our fat. When clinical grade, this diverse mix of cells are called Adipose-Derived Regenerative Cells (ADRCs).
In other words, there is a mixed population of stem cells and other regenerative cells in our fat. When clinical grade, this diverse mix of cells are called Adipose-Derived Regenerative Cells (ADRCs).