Why Adipose Tissue?
The Skinny on Fat
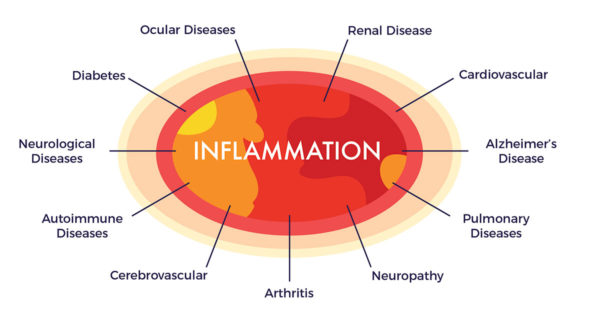 For thousands of years, people who would now be considered “overweight” were admired. To be large was a sign of prosperity and was associated with fertility as well as beauty, as demonstrated by the heavy set women featured in important works of art over many centuries. It is only in contemporary times that thin became in. This cultural shift may have occurred, in part, when medical research implicated obesity in a broad spectrum of inflammatory diseases.
For thousands of years, people who would now be considered “overweight” were admired. To be large was a sign of prosperity and was associated with fertility as well as beauty, as demonstrated by the heavy set women featured in important works of art over many centuries. It is only in contemporary times that thin became in. This cultural shift may have occurred, in part, when medical research implicated obesity in a broad spectrum of inflammatory diseases.
That doesn’t mean all fat (medically known as adipose tissue) is bad by any stretch. In fact, it is now well-appreciated that adipose is an important organ of a complex network, possessing regenerative capabilities[1] [2] and participating in the regulation of a variety of diverse biological functions.[3]
What is Fat Composed Of?
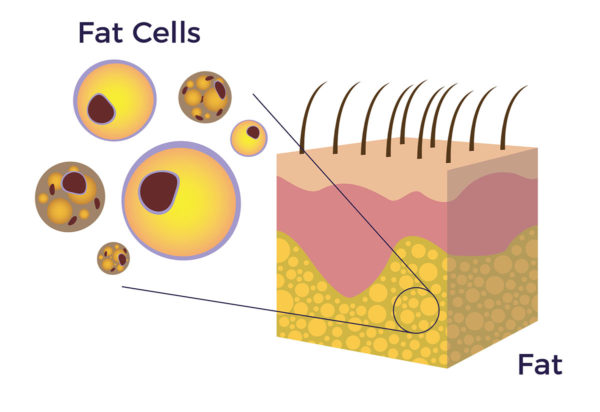 The word “adipose” comes from Latin from adeps, adip- ‘fat.’ Adipose is a loose connective tissue composed of fat cells (adipocytes). Connective tissue does just what its name implies—it connects things in our body together.
The word “adipose” comes from Latin from adeps, adip- ‘fat.’ Adipose is a loose connective tissue composed of fat cells (adipocytes). Connective tissue does just what its name implies—it connects things in our body together.
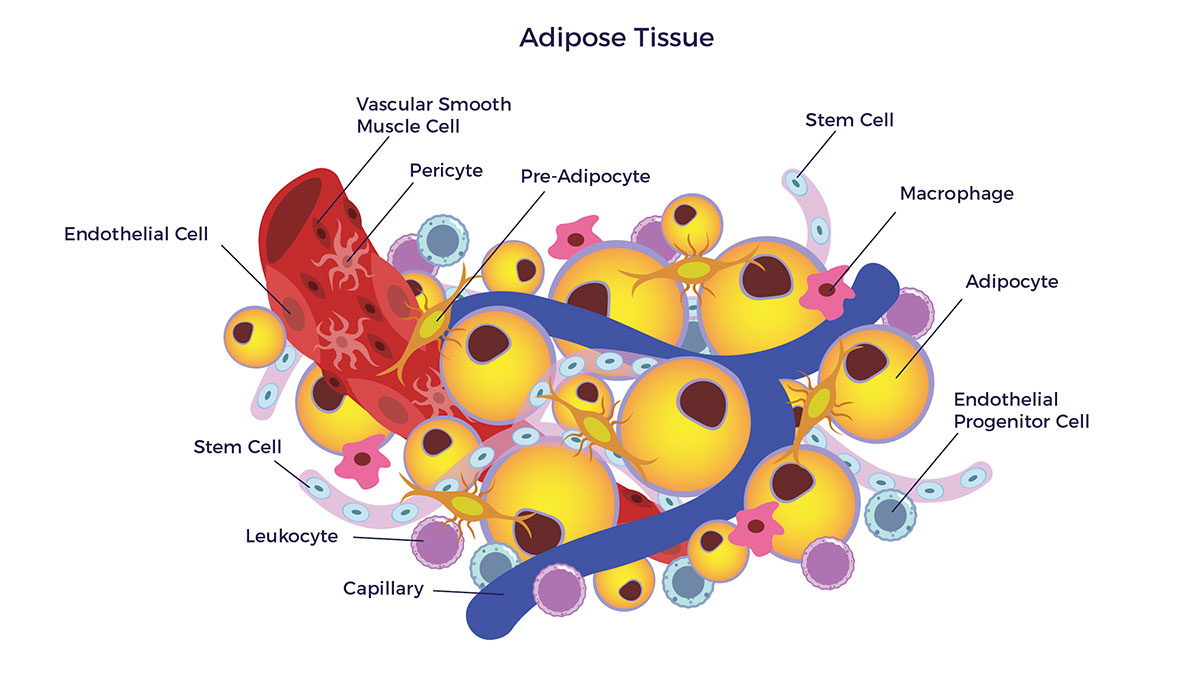
Although fat is the main component found in the tissue, there are nerves as well as capillaries intermingled in that tissue. The cells that reside on the inner lining of those capillaries (endothelium) are most relevant to cell therapy and are known as adipose-derived stem and regenerative cells (ADRCs).
The Breakdown: Adipose Stem and Regenerative Cells
 The regenerative cells in fat were first discovered in 1964 by Martin Rodbell, using an enzyme and a centrifuge. Research on adult stem cells took a quantum leap forward in 2001 when Patricia Zuk PhD, Dr. Marc Hedrick and others working in the labs of UCLA, published a paper in Tissue Engineering discussing their discovery of mesenchymal stem cells (MSCs) and other regenerative cells in our fat.[4] With that, a new era in medicine had begun. Since that seminal paper’s publication, investigators have published over 85,000 papers discussing adipose-derived stem cells (ADSCs). That is an average of 11 new publications per day over the past 22 years. The publishing rate has accelerated to 36 per day, nearly four times the historical average.
The regenerative cells in fat were first discovered in 1964 by Martin Rodbell, using an enzyme and a centrifuge. Research on adult stem cells took a quantum leap forward in 2001 when Patricia Zuk PhD, Dr. Marc Hedrick and others working in the labs of UCLA, published a paper in Tissue Engineering discussing their discovery of mesenchymal stem cells (MSCs) and other regenerative cells in our fat.[4] With that, a new era in medicine had begun. Since that seminal paper’s publication, investigators have published over 85,000 papers discussing adipose-derived stem cells (ADSCs). That is an average of 11 new publications per day over the past 22 years. The publishing rate has accelerated to 36 per day, nearly four times the historical average.
Whereas many stem cell researchers isolate and grow (in culture) the mesenchymal stem cells (MSCs) from bone marrow, umbilical cord and other tissues, it has been found that freshly prepared autologous (from self) contains a mixed population of both stem cells and other regenerative cells. It is this mixed population which we believe has the greatest potential to improve symptoms, function and quality of life for patients suffering from a broad range of chronic degenerative diseases. [5] [6] [7] We call this rich, diverse mixture adipose-derived stem and regenerative cells (ADRCs).
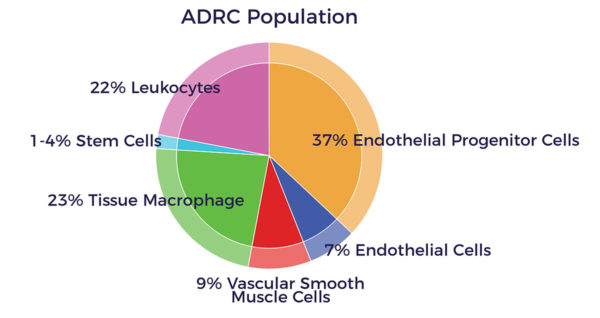 There are many different regenerative cell types found in ADRCs, including:
There are many different regenerative cell types found in ADRCs, including:
Endothelial Cells (ECs) – Cells which line the inside of every blood vessel and regulate exchanges between the bloodstream and the surrounding tissues. Signals from endothelial cells organize the growth and development of connective tissue (called the endothelium) that forms the surrounding layers of the blood vessel wall. ECs also line the lymphatic vessels that are part of our immune system and compose the blood-brain-barrier, which functions to protect the brain from substances that can disturb neural function.
Endothelial Progenitor Cells (EPCs) – Cells which play a role in the regeneration of the endothelial lining of blood vessels. They also have the ability to form stable blood vessels.
Leukocytes – A type of white blood cell that circulates in the blood and body fluids and is involved in counteracting foreign substances and disease.
Macrophage (literally “big eater”) – A type of mobile white blood cell that cleans the body of unwanted microscopic particles, such as bacteria and dead cells. Macrophage 1 (M1s) are inflammatory, whereas M2s are anti-inflammatory. ADRCs have M2s and also convert M1s to M2s.
Pericytes – A cell of the connective tissue that “wraps around” endothelial cells found in capillaries or other small blood vessels. Pericytes are thought to be pre-mesenchymal stem cells and regulate the blood-brain-barrier.
Vascular Smooth Muscle Cells (VSMCs) – Cells which make up normal blood vessel walls, provide structural integrity and regulate the diameter by contracting and relaxing dynamically in response to stimuli affecting the diameter of blood vessels (and hence blood pressure).
Mesenchymal Stem Cells (MSCs) – The basic building block cells in the body, capable of differentiating (turning into) other cell types, and making more of themselves. Current research tells us that the therapeutic benefits of MSCs are largely from what these cells do (as opposed to what they become) in terms of secreting key bioactive chemicals for repair.
Translating Therapeutic Benefits
In the presence of a chronic condition or disease, ADRCs have the power to set in motion a process of repair by:
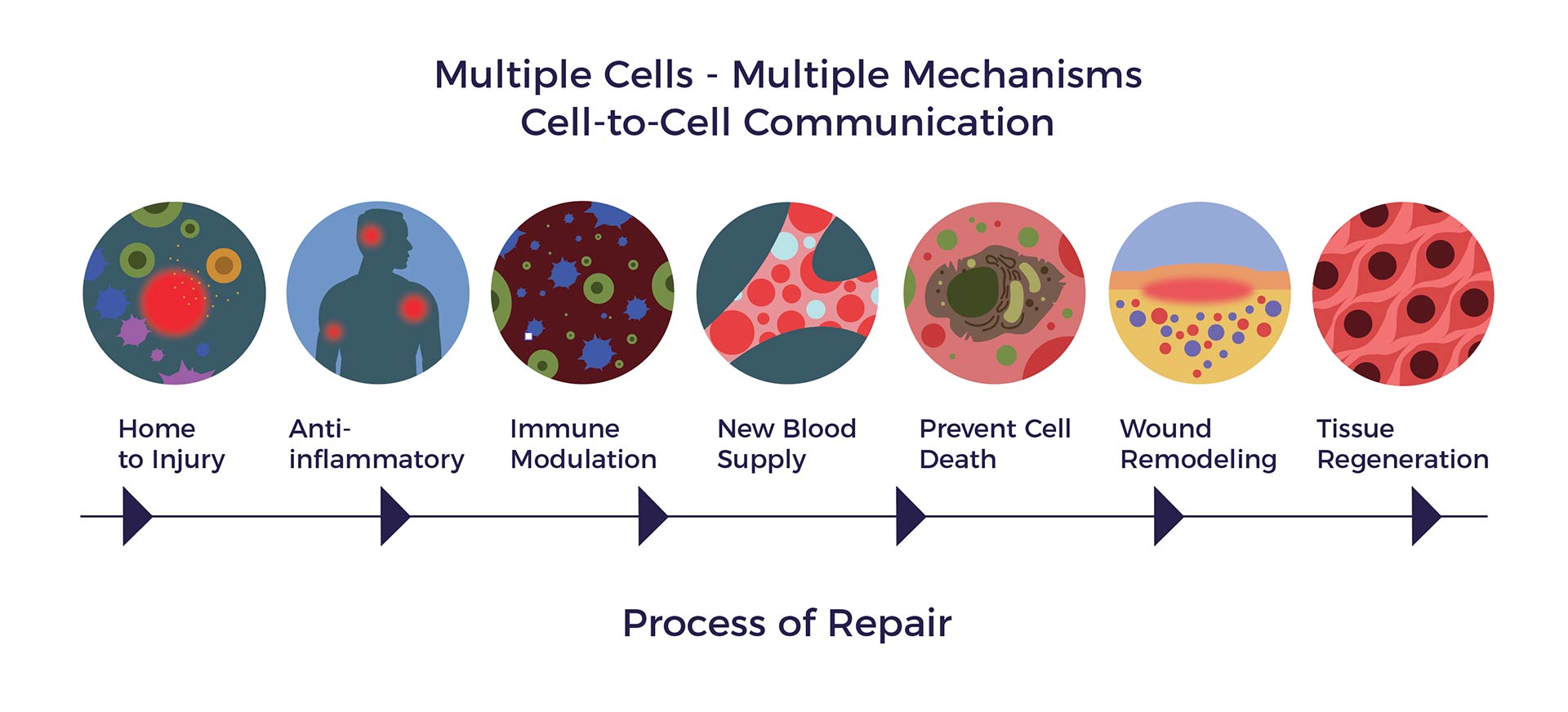
- Reducing inflammation
- Modulating abnormal immune responses
- Stimulating new blood vessel growth
- Preventing programmed cell death
- Secreting beneficial proteins and chemicals necessary for repair
- Reversing scar
- Regeneration of healthy tissue
Adult stem cells from different cells sources work for different indications including umbilical cord stem cells and bone marrow for certain blood cancers. Bone marrow stem cells have been shown to be most effective in orthopedic and cardiac cell therapy when used in middle age or younger due to their declining number and potency as we age. Conversely, ADRCs are accessible, abundant and potent later in life and hence are best suited for age-related degenerative diseases.
[1] P Tonnard et al Nanofat Grafting: Basic Research and Clinical Applications Plastic and Reconstructive Surgery October 2013
[2] C Tremolada et al Adipose Mesenchymal Stem Cells and Regenerative Adipose Tissue Graft (LipogemsÔ) for Musculoskeletal Regeneration European Journal of Musculoskeletal Diseases Vol. 3, no. 2, 0-0 (2014) 57
[3] M Cohleo et al Biochemistry of Adipose Tissue: An Endocrine Organ Arch Med Sci 2013; 9, 2: 191-200
[4] PA Zuk et al Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng 2001
[5]JK Fraser PhD and S. Kesten MD Autologous Adipose Derived Regenerative Cells: A platform for therapeutic applications Advanced Wound Healing Surgical Technology International XXIX
[6] A Nguyen, A et al Stromal vascular fraction: A regenerative reality? Part 1: Current concepts and review of the literature Journal of Plastic, Reconstructive & Aesthetic Surgery (2016) 69, 170e179
[7] Guo et al Stromal vascular fraction: A regenerative reality? Part 2: Current concepts and review of the literature Journal of Plastic, Reconstructive & Aesthetic Surgery (2016) 69, 180e188
