AMBROSE Cell Therapy for Orthopedics
Arthritis, back and neck pain, joint discomfort and sports injuries account for majority of Americans’ healthcare concerns. In a recent report from the American Academy of Orthopedic Surgeons, it was reported that over 126 million adults in the United States live with a musculoskeletal condition such as:
- Arthritis
- Back and neck pain
- Joint pain
- Orthopedic injury
At AMBROSE, adult stem cells derived from the adipose tissue (fat) are put to work to accelerate healing. Cell therapy for orthopedic pain focuses both on local joint dysfunction at the site of injury, as well as systemically to address any potentially underlying inflammatory-immune response which may be perpetuating or worsening the condition.
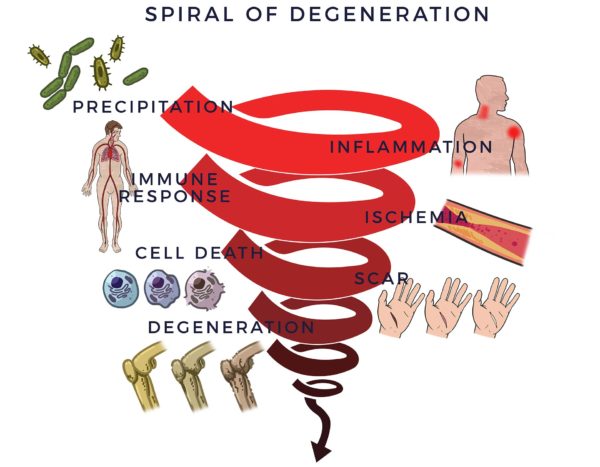
Spiral of Degeneration in Bones, Joints and Muscles
Musculoskeletal pain can be the product of acute injury, gradual wear, or both. Orthopedic degeneration generally begins with a trigger such as a trauma, wear and tear that becomes damaging, lifestyle choices, hereditary factors or any combination of thereof. This trigger is followed by an inflammatory response. This type of inflammation (acute) is essential for repairing the body, and is usually short-lived, disappearing once the healing process has taken place.
Inflammation becomes problematic when it lingers, becoming chronic, and affects the entire body, becoming systemic. Chronic, low-level systemic inflammation from various causes can play a contributing or lead role in the development of pain and dysfunction of the musculoskeletal system.[1] Further, systemic inflammation is a common factor in diseases of aging including those related to the bones and joints.[2] Research into diseases involving neck and back pain as well as sciatica has shown that inflammation is involved in the process of spinal degenerative diseases as well.[3] [4]
Chronic inflammation begins a detrimental process by first recruiting the immune system, whose usual job it is to fight infections and other disease processes so as to assist healing. When the cells in the immune system (immune cells) sense the inflammation, they send out troops of anti-inflammatory “cytokines” (bioactive molecules) to fight them off. When this process goes out of control, it is called an inflammatory-immune response.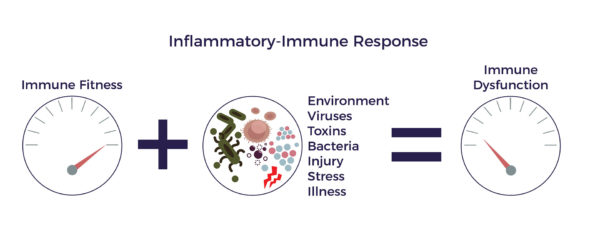
The inflammatory-immune response is tantamount to having a backseat driver who is chronically overreacting while “helping” you drive your car, which then leads to reduced blood flow (ischemia). Without a sufficient flow of oxygen and nutrient-rich blood to keep bones and joints healthy, cells die off, discs can bulge or herniate, the spinal column can narrow and begin to press on nerves, and the muscles, tendons and ligaments will weaken. Scars and bone spurs replace healthy tissue.
As we age the common denominators of chronic degenerative disease, which we refer to as the Spiral of Degeneration, can take hold throughout the musculoskeletal system, leading to debilitating pain, dysfunction and diminished quality of life.
Process of Repair in Joints
While adipose-derived stem and regenerative cells (ADRCs) have the capacity to regenerate healthy tissue, there are a vast number of additional therapeutic benefits these cells are capable of by means of what they do as opposed to merely what they become.
Through a mechanism of cell-to cell communication known as the paracrine effect, ADRCs recruit “repairmen” at the site of pain or injury—resident stem cells—to get back on the job and do their part. As an extended team, they work to decrease inflammation and overactive immune responses, to increase circulation with new blood vessel growth, prevent further cell death, decrease scar size and regenerate healthy tissue as validated by a recent study with MRI imaging, demonstrating the potential of cartilage regeneration.[5] [6]
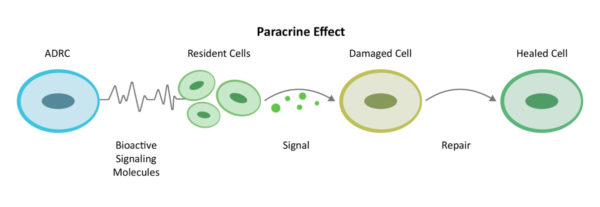
We call this the Process of Repair as it involves the multiple mechanisms of action that are needed to repair tissue, reduce both systemic and local inflammation and bring the inflammatory immune response back to balance and thus improve overall joint health and function.
Functional Joint Unit
A joint is defined as the juncture where two or more bones come together for the purpose of movement or for stabilization. Normal joint function is defined as a joint’s ability to move throughout its range of motion, bear weight and perform work. That includes how far it should be able to flex, extend or rotate. The ability to bear weight or to resist pressure opposing the action of the joint are other aspects of joint function.

As a further example, all of the structures of the hip are like spokes on a wheel to stabilize the pelvis to the femur (hip bone), hence the contribution to the functions of the hip joint. That’s why we call this a “functional unit,” as all these components both physiologically and functionally stabilize, move and support the hip joint.
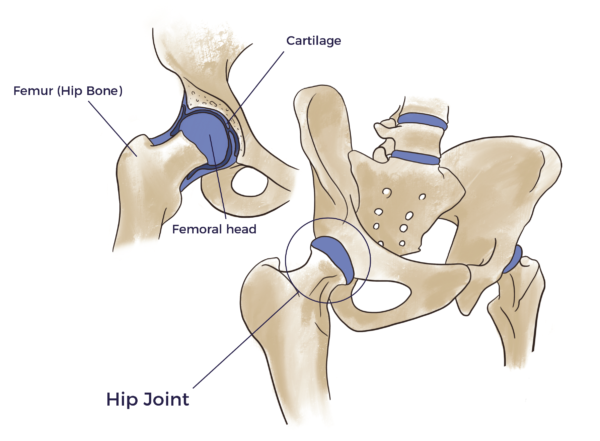
When a joint becomes dilapidated it stresses everything around it. The stress leads to inflammation which then leads to degeneration and arthritis in other compartments. Surgeries of joints are done to repair the main structural culprit such as a partial or full tear of cartilage or tendon. In the case of a “bone-on-bone” joint, it is replaced in part or entirely with a man-made implant. Though appropriate in some cases, these solutions can be limited as a joint can have many bad actors contributing to the pain. For that reason, AMBROSE pursues a global approach by treating any pain-generating abnormality in all of the compartments of each symptomatic joint as located at the point of care by ultrasound imaging.
Our Orthopedic Approach
AMBROSE Cell Therapy for orthopedic issues treats the functional joint unit, including all component muscles, tendons, ligaments and so forth that contribute to stability, mobility and overall pain-free function.
While the main culprit in a joint may be a torn tendon, cartilage or muscle, our orthopedic specialists inject all of the pain-generating abnormalities in the functional unit. This is best facilitated by the use of point-of-care diagnostic ultrasound imaging to view all contributing abnormalities. Ultrasound guided injections enable our medical team to precisely deliver the cell therapy injections to treat each component individually and provide live visual feedback in real time ensuring we have.
Further, whereas in the not too distant past arthritis itself was considered a “wear and tear” disease, and the cause of the symptoms associated with it were believed to be strictly structural, it is now well appreciated that age-related inflammation and immune system dysfunction are culprits that contribute to the symptoms of degenerative joint diseases.
AMBROSE Cell Therapy for Orthopedic Pain and Dysfunction
The scientists researching adult stem cell therapy for degenerative joint diseases now widely recognize that ADRCs have the potential to reduce inflammation, rebalance the immune system and initiate a process of repair in arthritis, back and neck pain or loss of function due to an orthopedic injury.[7] [8] [9]
AMBROSE Cell Therapy represents a minimally invasive option for patients with degenerative orthopedic conditions. Please contact us for more information about treatment, candidacy and how to become a patient.
[1] J Gallo Inflammation and its resolution and the musculoskeletal system J Orthop Translat. 2017 July; 10: 52–67
[2] C. Franceschi and J. Campisi Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases J Gerontol A Biol Sci Med Sci 2014 June;69(S1): S4–S9
[3] M. Shamji et al Proinflammatory Cytokine Expression Profile in Degenerated and Herniated Human Intervertebral Disc Tissues Arthritis Rheum. 2010 July; 62(7): 1974–1982
[4] J Gallo Inflammation and its resolution and the musculoskeletal system J Orthop Translat. 2017 July; 10: 52–67
[5] A Bowles et al Immunomodulatory Effects of Adipose Stromal Vascular Fraction Cells Promote Alternative Activation Macrophages to Repair Tissue Damage. Stem Cells, 2017 Aug 12
[6] D Hudetz et al The Effect of Intra-articular Injection of Autologous Microfragmented Fat Tissue on Proteoglycan Synthesis in Patients with Knee Osteoarthritis Genes 2017, 8, 270
[7]JK Fraser PhD and S. Kesten MD Autologous Adipose Derived Regenerative Cells: A platform for therapeutic applications Advanced Wound Healing Surgical Technology International XXIX
[8] A Nguyen, A et al Stromal vascular fraction: A regenerative reality? Part 1: Current concepts and review of the literature Journal of Plastic, Reconstructive & Aesthetic Surgery (2016) 69, 170e179
[9] Guo et al Stromal vascular fraction: A regenerative reality? Part 2: Current concepts and review of the literature Journal of Plastic, Reconstructive & Aesthetic Surgery (2016) 69, 180e188