AMBROSE Cell Therapy for Diabetes
In 2001, a new field of research in health science emerged when Patricia Zuk Ph.D., Marc Hedrick, M.D. and others published a paper in Tissue Engineering discussing their discovery that adult stem cells (mesenchymal stem cells, MSCs) that repair diseased and damaged tissues and organs reside along with other regenerative cells in our fat (adipose tissue).[1]
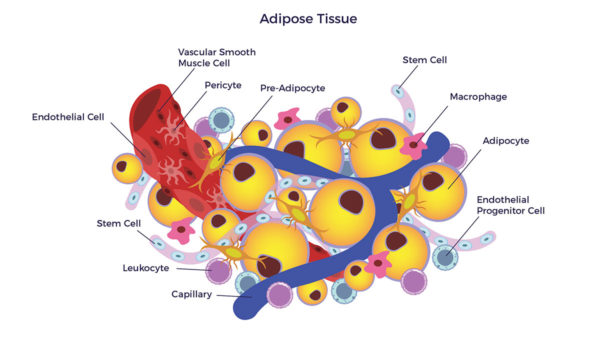 Since that publication over 11,000 papers have been published on the subject of adipose-derived stem and regenerative cells (ADRCs). [2] [3] [4] An important aspect of that research has been the potential benefit in symptoms, function and quality of life that ADRCs can have for patients with Diabetes Mellitus (DM).
Since that publication over 11,000 papers have been published on the subject of adipose-derived stem and regenerative cells (ADRCs). [2] [3] [4] An important aspect of that research has been the potential benefit in symptoms, function and quality of life that ADRCs can have for patients with Diabetes Mellitus (DM).
Understanding Diabetes
The first recognizable reports of Type 1 Diabetes Mellitus—a condition presenting in children or young adults that can have life threatening consequences—appeared towards the end of the 19th century. Interestingly, it was not until the 1970s that T1DM was recognized as an autoimmune disease. Type 1 diabetes is a chronic health condition in which one’s pancreas, a gland that lies in the abdomen behind the stomach, is deficient in producing enough of the hormone insulin. Insulin drives glucose (sugar) into the cells and modulates fat metabolism.
The pancreas contains clusters of cells that produce hormones. Alpha cells make the hormone glucagon, which raises the glucose level in the blood. Beta cells make the hormone insulin, which lowers the glucose level. In Type 1 diabetes, the body’s immune system mistakenly destroys the beta cells. This causes the pancreas to lose the ability to make
Type 2 Diabetes Mellitus (T2DM) is a chronic condition in which one’s body develops resistance to insulin, and blood sugar levels become very high as a result. T2DM is also now widely recognized to have an autoimmune component.[5]
ADRCs and Diabetes
ADRCs are akin to having a highly personalized biologic “fire, rescue and repair” crew. They wait quietly for a sign of trouble—inflammation—and home to that site to do their jobs. The scientists researching the cell types contained in the ADRC population have demonstrated experimentally (in small and large animals) as well as in human clinical studies that these cells are safe and have been effective in improving the function of the beta cells in the pancreas responsible for insulin secretion. Adipose-derived stem cells (ADSCs) have also been reported to rebalance the immune system (immune-modulation) after an abnormal immune response more effectively than stem cells from the bone[6] [7]
Spiral of Degeneration
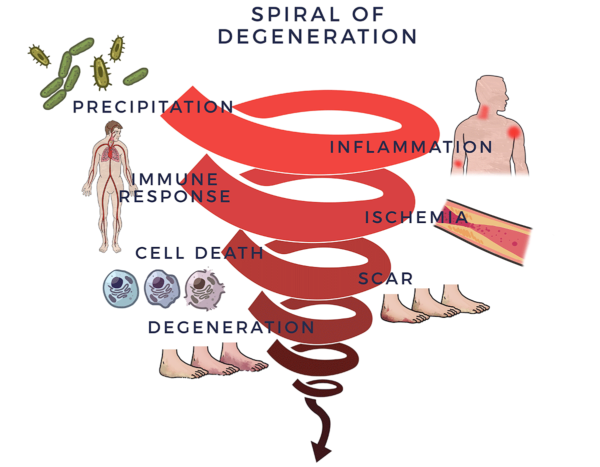
Inflammation in the pancreas can be triggered by hereditary factors, a trauma, infection, environmental toxins, lifestyle choices (e.g. alcohol abuse in adults), stress or a combination of those bad actors.[8] Initially, acute inflammation is essential for repairing the body, and is usually short-lived, disappearing once the healing process has taken place. There is another type of inflammatory response, sometimes called chronic or systemic inflammation, which becomes problematic.[9] Systemic inflammation is a common factor in diseases of aging. This covers a broad spectrum of severe, debilitating and, sometimes, life-threatening conditions including diabetes.[10]
Chronic inflammation begins a vicious detrimental process. It recruits the immune system, which exists to fight infections and other disease processes as well as to guard the body and assist healing. When the immune system senses an enemy, troops of molecules called “cytokines” are sent out to fight it off. When this process goes out of control, it is called an inflammatory-immune response.
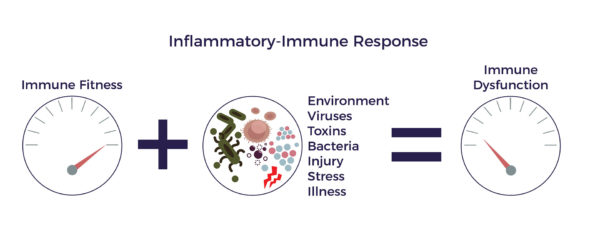 An inflammatory-immune response is tantamount to having a backseat driver who is chronically overreacting while “helping” you drive your car. Although the specific metabolic pathways are different for T1DM and T2DM, they both end up promoting die-off of pancreatic beta cells.[11] We call this the Spiral of Degeneration.
An inflammatory-immune response is tantamount to having a backseat driver who is chronically overreacting while “helping” you drive your car. Although the specific metabolic pathways are different for T1DM and T2DM, they both end up promoting die-off of pancreatic beta cells.[11] We call this the Spiral of Degeneration.
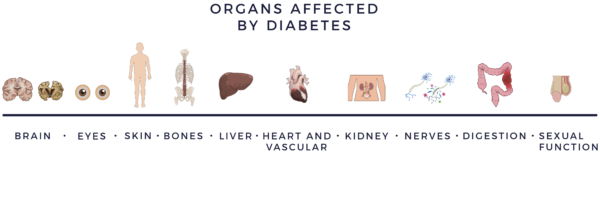
The Spiral is a useful framework for exploring the key factors at play in chronic diseases such as diabetes, though each step of degeneration in the Spiral may vary in terms of severity and sequence from person to person. Likewise, as the factors in the Spiral progressively worsen in diabetes sufferers, end organ damage can also vary. Diabetes is known to cause degeneration across many areas of the body from the brain and eyes to the heart, kidneys, skin, nerves and more.
Process of Repair
Through a mechanism of cell-to cell communication called paracrine signaling, ADRCs mobilize nearby cells to work more efficiently. To continue with the ‘fire, rescue and repair crew’ analogy, ADRCs recruit inactive stem cells in the region, getting them back on the job and doing their part.
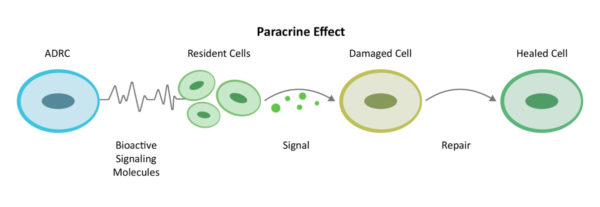 They first decrease inflammation and the overactive immune responses. Once the backseat driving diminishes, the stem and regenerative cells increase circulation with new blood vessel growth, prevent further accelerated cell death, decrease scar size and regenerate healthy tissue and nerves. This is how the body naturally heals itself– sometimes additional stem cells are needed as reinforcements. We call this the Process of Repair.
They first decrease inflammation and the overactive immune responses. Once the backseat driving diminishes, the stem and regenerative cells increase circulation with new blood vessel growth, prevent further accelerated cell death, decrease scar size and regenerate healthy tissue and nerves. This is how the body naturally heals itself– sometimes additional stem cells are needed as reinforcements. We call this the Process of Repair.
 In T1DM, this process can lead to regeneration of islet cells as well as the repair of nerves that have been damaged leading to diabetic neuropathy.
In T1DM, this process can lead to regeneration of islet cells as well as the repair of nerves that have been damaged leading to diabetic neuropathy.
AMBROSE Cell Therapy for Diabetes
AMBROSE Cell Therapy represents a minimally invasive option to improve symptoms, function and quality of life for patients with diabetes.
The AMBROSE treatment approach includes intravenous infusion of ADRCs to address the pancreas through the homing mechanism of the cells as well as the systemic inflammation and immune dysregulation that has been implicated in this condition.
Please contact us for more information about treatment, candidacy and how to become a patient.
[1] PA Zuk et al Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng 2001
[2]JK Fraser PhD and S. Kesten MD Autologous Adipose Derived Regenerative Cells: A platform for therapeutic applications Advanced Wound Healing Surgical Technology International XXIX
[3] A Nguyen, A et al Stromal vascular fraction: A regenerative reality? Part 1: Current concepts and review of the literature Journal of Plastic, Reconstructive & Aesthetic Surgery (2016) 69, 170e179
[4] Guo et al Stromal vascular fraction: A regenerative reality? Part 2: Current concepts and review of the literature Journal of Plastic, Reconstructive & Aesthetic Surgery (2016) 69, 180e188
[5] Winer, DA, et al, “B cells promote insulin resistance through modulation of T cells and production of pathogenic IgG antibodies.” Nature Medicine, Published online: 17 April 2011
[6] K Timper et al Human adipose tissue derived mesenchymal stem cells differentiate into insulin, somatostatin, and glucagon expressing cells. Biochem Biophys Res Commun 2006; 341: 1135-1140
[7] S M Melief et al Adipose Tissue-Derived Multipotent Stromal Cells Have a Higher Immunomodulatory Capacity Than Their Bone Marrow-Derived Counterparts STEM CELLS TRANSLATIONAL MEDICINE 2013;2:455–463
[8] M Nygren et al Experience of a serious life event increases the risk for childhood type 1 diabetes: the ABIS population-based prospective cohort study Springer-Verlag Berlin Heidelberg 2015
[9] S. Amor Inflammation in neurodegenerative diseases Immunology, 129, 154–169
[10] C. Franceschi and J. Campisi Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases J Gerontol A Biol Sci Med Sci 2014 June;69(S1): S4–S9
[11] Rojas J, et al “Review Article – Pancreatic Beta Cell Death: Novel Potential Mechanisms in Diabetes Therapy” Journal of Diabetes Research, Volume 2018, Article ID 9601801, 19 pages.