AMBROSE Cell Therapy for Autoimmune Diseases
Since the 1970s, the use of stem cells to treat autoimmune (AI) disease has been an area of intense research. Today, using patients’ own stem cells, new treatment opportunities have been made possible outside of the research setting. AMBROSE Cell Therapy brings patients a safe therapeutic approach beyond immunosuppressant drugs – drugs that can have potentially devastating long-term effects.
There are at least 100 autoimmune diseases, some of the most prevalent being:
- Diabetes
- Rheumatoid Arthritis (RA)
- Multiple Sclerosis (MS)
- Lupus (SLE)
- Psoriasis and psoriatic arthritis
- Crohn’s and other inflammatory bowel diseases
The complex nature of the immune system includes a wide variety of responses and triggers that sometimes turn against one’s own body, resulting in autoimmune disorders. Today, an estimated 50 million Americans live with conditions involving an inflammatory immune response, and women are disproportionately affected.[1]
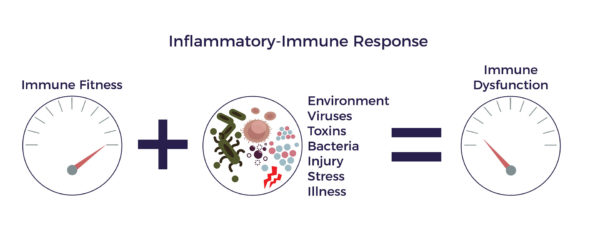
Inflammatory-Immune Response
Inflammation can be triggered by trauma, infection, environmental toxins, lifestyle choices (e.g., smoking), hereditary factors or a combination of those bad actors. The cells in the immune system are there to guard the body, fight infections and other disease processes, and to assist healing. When they sense the enemy, they send out defensive troops of pro-inflammatory molecules. This immediate type of inflammation is essential for repairing the body and fighting infection. It is usually local and short-lived, disappearing once the healing process has taken place.
Inflammation is only problematic when it lingers, becoming chronic, and affects the entire body, becoming systemic. Chronic, systemic inflammation is the hallmark of autoimmune disease.[2] In AI, the immune response is hijacked. The normal orderly, limited immune process goes out of control, into a damaging inflammatory-immune response. This starts a vicious cycle that promotes chronic and systemic inflammation.
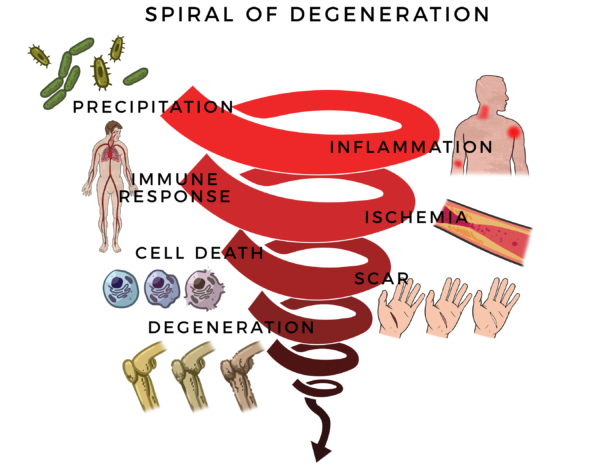
The inflammatory-immune response is tantamount to having a backseat driver who is chronically overreacting while ‘helping’ you drive. It leads to reduced blood flow. Without good circulation, cells die off and scars form; eventually, tissues and then organs degenerate. AI diseases can destroy joints, intestines, connective tissue, internal organs, nerves and brain cells. We call this the Spiral of Degeneration.
Autoimmune diseases involve a chronic systemic inflammatory-immune response perpetuating the Spiral. This can progress to involve the lungs, heart, kidneys, brain and liver, and even predispose to cancer. Many patients have two or more autoimmune conditions concurrently.
Stem Cell Repair
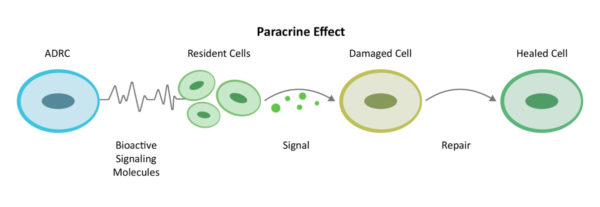
Ones’ own fat (adipose tissue) is a rich storehouse of stem and regenerative cells. In the early research days, stem cells were thought to only have the function of regenerating healthy tissue and nerves. But it is now known that adipose-derived stem and regenerative cells (ADRCs) promote tissue repair in many ways.
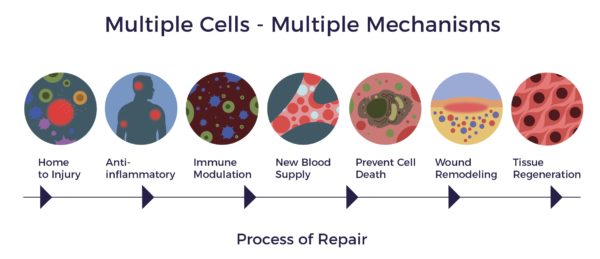
Through a mechanism of cell-to cell communication, ADRCs work to mobilize nearby cells to work more efficiently. ADRCs assemble an extended team by recruiting additional ‘repairmen’ at the site of disease or injury, stimulating local stem cells to get back on the job and do their part to decrease inflammation and quiet down the overactive immune responses. Once the backseat driving diminishes, the stem and regenerative cells continue their work by increasing circulation with new blood vessel growth, preventing further cell death, and decreasing scar size. Finally stem cells become the building blocks for the regeneration of healthy tissue and nerves.[3][4][5]
 These actions describe how the body naturally heals – sometimes it just needs reinforcements. We call this the Process of Repair, as it involves the multiple mechanisms of action that are needed to bring the systemic inflammation and immune system back to balance.[6]
These actions describe how the body naturally heals – sometimes it just needs reinforcements. We call this the Process of Repair, as it involves the multiple mechanisms of action that are needed to bring the systemic inflammation and immune system back to balance.[6]
In addition to modulating the inflammatory immune response in AI, the healing process can extend to include repair actions in organs affected by autoimmune diseases. New blood vessels can form and new neurons in the brain can be generated as a result of the multiple activities the ADRCs perform. There can be regeneration of the myelin sheathing that insulates the nerves, of connective tissue that supports muscle and bone, and the cartilage in joints.[7]
AMBROSE Cell Therapy for Autoimmune Diseases
Adipose-Derived Stem and Regenerative Cells (ADRCs) have the potential to help patients living with autoimmune diseases to improve symptoms, function and quality of life. ADRCs are a diverse population of cells that have multiple actions to bring about healing and repair. Scientists researching adult stem cell therapy for autoimmune diseases now widely recognize that ADRCs reduce inflammation and rebalance the immune system in initiating the process of repair.[8] These cells are akin to having your own, personalized biologic repair crew. Waiting quietly for a sign of trouble—inflammation—they migrate to the damaged sites to do their jobs.[9]
AMBROSE Cell Therapy represents a minimally invasive option for patients with autoimmune diseases. Please contact us for more information about treatment, candidacy and how to become a patient.
[1] Ortona E, Pierdominici M, Maselli A, Veroni C, Aloisi F, Shoenfeld Y. Sex-based differences in autoimmune diseases. Ann Ist Super Sanita. 2016 Apr-Jun;52(2):205-12.
[2] Pohl D, Benseler S. Systemic inflammatory and autoimmune disorders. Handb Clin Neurol. 2013;112:1243-52.
[3] Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, Benhaim P, Lorenz HP, Hedrick MH. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7(2):211–28.
[4] Zuk PA, Zhu M, Ashjian P, De Ugarte DA, Huang JI, Mizuno H, Alfonso ZC, Fraser JK, Benhaim P, Hedrick MH. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell. 2002;13(12):4279–95.
[5] Nakagami H, Maeda K, Morishita R, Iguchi S, Nishikawa T, Takami Y, Kikuchi Y, Saito Y, Tamai K, Ogihara T, Kaneda Y. Novel autologous cell therapy in ischemic limb disease through growth factor secretion by cultured adipose tissue-derived stromal cells. Arterioscler Thromb Vasc Biol. 2005;25(12):2542–7.
[6] Qi K, Li N, Zhang Z, Melino G. Tissue regeneration: The crosstalk between mesenchymal stem cells and immune response. Cell Immunol. 2018 Apr;326:86-93.
[7] Gimble JM, Katz AJ, Bunnell BA. Adipose-Derived Stem Cells for Regenerative Medicine. Circ Res. 2007 May 11; 100(9): 1249–1260.
[8] Volarevic V, Gazdic M, Simovic Markovic B, Jovicic N, Djonov V, Arsenijevic N. Mesenchymal stem cell-derived factors: Immuno-modulatory effects and therapeutic potential. Biofactors. 2017 Sep 10;43(5):633-644.
[9] Eggenhofer E, Luk F, Dahlke MH, Hoogduijn MJ. The life and fate of mesenchymal stem cells. Front Immunol. May 2014, Volume 5, Article 148:1-6.